
Tracheostomy 101 2.0 CE Hours
Course Objectives:
- Describe the anatomy of the trachea.
- List indications for a tracheostomy.
- List the contraindications for a tracheostomy
- Discuss the surgical steps required to perform a tracheostomy
- Explain the complications and weaning off a tracheostomy
Abstract
Tracheostomy is a common surgical procedure performed by surgeons to help create a surgical airway. The terms tracheotomy and tracheostomy both have the same meaning and are often used interchangeably. Tracheostomy is generally performed in the cervical neck region in patients who are not able to weaned off the mechanical ventilator or in those patients who need aggressive clearing of very thick and viscous oral secretions that block the upper airways. Once an opening is created in the upper trachea, a specially designed cannula is inserted into the airway. It is secured with sutures. It usually takes 1-2 weeks for a mature tract to form and during this time, great care must be taken to avoid dislodgement of the cannula.
Tracheostomy is a very common surgical procedure performed in most health care institutions. The ultimate aim of the procedure is to provide the patient with a patent airway. Tracheostomy is usually a temporary procedure in most patients but in some rare cases, the surgeon may perform a permanent tracheostomy. Tracheostomy is not a new procedure at all. It was performed in a crude form nearly a century ago for the treatment of diphtheria and neck trauma. Often in traumatic neck or facial cases, the throat was slashed with a knife. Due to lack of anesthesia and proper surgical instruments, this often led to death of patients from exsanguinating bleeding, rather than from the illness. The other reason why tracheostomy was such a dreaded procedure many centuries ago because the people who performed the procedure had little knowledge about the anatomy, had very poor surgical technique and there was no anesthesia and the equipment was crude. A lot has changed in the last half a century, which has made tracheostomy a much safer procedure today. There are much better instruments available, the surgeons know the anatomy, only qualified surgeons do the procedure and the anesthesia is excellent. Today, tracheostomy is no longer considered a major procedure and now done in a minor operating room. However, tracheostomy has the potential to be a complicated procedure if one deviates from the surgical anatomy and rushes the procedure. Catastrophic bleeding can occur and within seconds the patient’s life can be jeopardized. A common reason for complication is not appreciating the tracheal anatomy and surgically deviating away from the midline.1-15
Indications for Tracheostomy
The primary reason for performing a tracheostomy is when the patient fails to be weaned off the endotracheal tube after 3-4 weeks. The patient shows little ability to be breathe on his own and rather than prolong the orotracheal tube intubation a tracheostomy is performed.
Tracheostomy may also be performed in a patient who has suffered a neurological event like a stroke and is unable to keep the upper airways patent.
People involved with midfacial trauma or have upper airway injury may also be candidates.
In some neurological disorders where the diaphragm or the phrenic is paralyzed, a permanent tracheostomy is needed.
Tracheostomy is sometimes performed in patients with severe epiglottis who have difficulty breathing and other head and neck infection where there is an imminent risk of airway blockage. Tracheostomy may sometimes be performed in patients with cancers of the oral cavity and pharynx. Today, with improved antibiotics and better ICU care the role of tracheostomy for managing diphtheria and epiglottis has diminished. In any case, in any patient admitted with epiglottitis or diphtheria, a tracheostomy set must be kept at the bedside.
In young children and neonates born with congenital disorders or malformations of the head and neck like a hemangioma or a large laryngeal mass, tracheostomy may sometimes be life saving. In very rare cases, a tracheostomy may be required in individual who has a foreign body stuck in the upper airways, and which cannot be retrieved with laryngoscopy.
Finally, when the individual has bilateral recurrent nerve injury or bilateral phrenic nerve paralysis, a permanent tracheostomy is needed. In the emergency room, the most common indication for a tracheostomy is mid facial or neck trauma. Almost any type of face and neck trauma that make breathing difficult nay be an indication for an immediate tracheostomy.
Sometimes fracture of the larynx, mandible or midface that can cause severe edema of the pharynx and upper airways mandate an immediate tracheostomy.
Other times when a tracheostomy is needed is in an individual with facial burns, anaphylaxis or lye injury. These conditions often lead to rapid swelling of the pharyngeal tissue leading to edema and blockage of the upper airways.
A very common reason for a tracheostomy in an ICU patient is to improve pulmonary toilet; some patients have a very weak cough and are unable to cough up their secretions. These individuals are prone to pulmonary aspiration because they are not able to cough up the oral secretions. These individuals often benefit from what is called a prophylactic tracheostomy. This helps the respiratory therapist easily remove the viscous thick tracheal secretions a lot easily.
Prophylactic tracheostomy is also sometimes done in patients who undergo a laryngectomy. The tracheostomy helps with healing and can be closed when the facial and neck edema and swelling have subsided. Finally, some patients with sleep apnea may benefit from a tracheostomy. However, a tracheostomy in these patients is only done after all other conservative methods of treatment have failed.
Tracheal Anatomy
The trachea is a hollow tube that links the cricoid cartilage of the larynx to the carina. It forms part of the airway conduction system brining air from the nose into the lungs. The trachea is composed of 15-20 C shaped rings, and made from cartilage. The trachea is membranous posteriorly but is formed of cartilage in the anterior portion. The tracheal rings are connected to each other via elastic connective tissue. The proximal or cervical trachea is in the midline of the neck but as it moves into the chest, the trachea moves slightly to the right as it enters the chest cavity. The opening of the larynx has a flap-like covering known as the epiglottis, which closes during swallowing to prevent aspiration. Because the tracheal blood supply is on the lateral side, dissection should NOT be performed in this location as it may easily lead to devascularization and necrosis of the tracheal cartilage.
The thoracic trachea passes over the aortic arch and bifurcates into the left and right main bronchi at the level of the 4th-6th intercostal space. This level of bifurcation is fairly constant and occurs at T4-T5. The trachea is designed in such a way that it will not collapse during expiration. The walls of the trachea are made of several layers that help keep the structure open and yet mobile. The inner mucosal lining of the trachea produces mucus, which traps debris and constantly flows upwards to towards the oral cavity where it is swallowed.
The recurrent laryngeal nerves run on the lateral aspects of the tracheoesophageal groove. The right recurrent laryngeal nerve is very close to the trachea and hence more vulnerable to injury if any dissection is done in this area. In young children, the trachea is intimately related to the aortic arch and its branches; extensive dissection in the anterior or superior mediastinum can lead to torrential bleeding if any of these vessels is injured. The thyroid gland sits on top of the trachea at the level of the second to third tracheal rings. Because the thyroid is a very vascular structure, good hemostasis is a requisite when performing a tracheostomy. Most surgeons prefer to stay in the midline during surgery because it is devoid of any major blood vessels. The esophagus runs behind the trachea.
Contraindications
Even though there are no absolute contraindications to performing a tracheostomy, the patient must have a normal coagulation profile. In patients who have malignancy of the head and neck, it is important to avoid manipulation of these tissues as it may seed tumor cells into the tracheal incision. The surgeon should never make the incision for a tracheostomy in the first tracheal ring as this can lead to subglottic stenosis. Tracheostomy is not a palliative procedure and should not be done in patients who are terminally ill or moribund. It is important for the healthcare workers to speak to the patient’s family and friends about the procedure and why it is done. Overall, tracheostomy is much better tolerated than an oral endotracheal tube. It permits the therapist to maintain good airway hygiene and remove the secretions. It should never be done just to keep a patient alive.
Timing of Surgery
Prior to a tracheostomy, the majority of patients are intubated and on a mechanical ventilator in the ICU. Only a few patients present to the Emergency room with upper airway obstruction who are in urgent need for a tracheostomy. There is no universal time when a patient should get a tracheostomy after he/she has been on the mechanical ventilator. However, most critical care experts consider that after 3-4 weeks, if the patient shows no signs of being weaned off the mechanical ventilator, a tracheostomy should be considered. All patients must be given every opportunity and ample time to determine if they can be weaned off the endotracheal tube. In very rare cases, a tracheostomy is done within a few days after orotracheal intubation-this scenarios is more likely in patients with severe head trauma or stroke who have little or no probability of coming off the ventilator. Most surgeons will not perform a tracheostomy in children for at least 4-5 weeks.
It is worth remembering that in a patient with prior oral endotracheal intubation, a tracheostomy is slightly easier to perform. Because the patient already has an oral tube in the trachea the surgeon and anesthesiologist feel confident that should anything untoward happen during the procedure, then the anesthesiologist can simply start ventilation via the endotracheal tube. Scenarios where a tracheostomy is often done immediately without prior oral intubation include patients with severe facial trauma, patients with upper airway obstruction (epiglottitis) or C spine fracture.
Most tracheostomies are done on an elective basis in a controlled environment with trained OR staff. Emergent tracheostomy or slash procedure is only done in dire circumstances, such as when a cricothyrotomy is impossible. Emergent tracheostomy is sometimes done in patients with acute respiratory distress from epiglottitis or foreign body obstruction. The procedure can be performed in the ER under local anesthesia, but it is vital that an anesthesiologist be present to monitor the airway and provide guidance. Most patients require some type of IV sedation or even the use of paralytic agents. Moreover, the surgeon should also have steady hands because a tracheostomy in a conscious patient is very stressful and demanding. There is little room for error and the procedure can be challenging. Emergent tracheostomy especially in the ED setting is often associated with extremely high morbidity and mortality and should be avoided if at all possible.
Preoperative Details
Like all surgery procedure, a valid informed consent must be obtained prior to the procedure. The general preoperative work up includes complete blood count, coagulation profile and a chest x-ray.
The Procedure
Even though tracheostomy is a minor surgical procedure it does require a great deal of care and thought. It is not a procedure that should be done in the ER or at the bedside if there is no surgery assistance. In the emergency room, there is usually poor lighting, the equipment may not all be there and sterility is always questionable. Further, in the ER, operating room trained nurses are not always present. Tracheostomy is a semi elective or elective procedure and it is almost never an emergency.
If possible, tracheostomy should be done on a semi-elective basis in the regular operating room. An anesthesiologist should always be present during the performance of a tracheostomy. The patient needs to have good intravenous access, and be monitored via an ECG, pulse oximetry and blood pressure.
Tracheostomy is done with the patient in a supine position and the neck slightly extended. In obese individuals or those with a short neck, a small roll can be placed under the neck for extension and bringing the neck forward. In awake individuals who are having a tracheostomy under only local anesthesia, the shoulder roll may not be well tolerated. In these individuals, the head of the bed may have to be elevated to bring the trachea forward. Too much extension of the neck should also be avoided as it stretches and narrows the diameter of the trachea. In addition, cervical neck extension especially in children can bring out the mediastinal trachea into the neck area. This can result in an inadvertent tracheostomy in the 4th or 5th ring, which is dangerously close to the innominate artery. This is a common mistake when performing tracheostomy in children.
Before making the incision, the entire neck and chest area should be draped and prepped. Prior to making the surgical incision, the surgeon should identify the anatomical landmarks-, which include the sternal notch, midline trachea and cricoid cartilage. Some surgeons infiltrate the skin and subcutaneous tissues with lidocaine containing epinephrine to achieve good hemostasis.
A small (2- to 3-inch) horizontal skin incision is usually made along the skin tension lines to afford good cosmesis. Because the skin around the neck is very vascular, complete hemostasis should be obtained before dissecting deeper in the tissues. The subcutaneous tissue can be incised using electrocautery. Once the platysma is reached, the trachea should be palpated. The neck muscles should then be opened up only in the midline and a retractor used to expose the thyroid gland. All small blood vessels the skin and subcutaneous tissues should be checked to ensure that there is no bleeding. All medium and large size blood vessel should be tied or clipped. The most critical part of surgery is to stay in the midline. Large blood vessels run on either side of the trachea and they can bleed profusely if injured. Once the strap muscles are retracted laterally, the thyroid isthmus comes into view.
In most people the thyroid isthmus is a narrow band of tissue but it still needs to be ligated with sutures and then cut. If the thyroid isthmic tissue is flexible and long, it can be retracted superiorly while performing the tracheostomy. However, do remember that it may interfere with the tracheostomy cannula in future. It can lead to torrential bleeding if injured. After the isthmus is ligated, the trachea is easily visualized and the 2nd cartilage ring can easily ne exposed. It is important to speak to the anesthesiologist at this point. The tracheostomy instruments should all be ready before an incision in the trachea is made. Once the tracheostomy tube is inserted, it should be secured with stitches to the skin. The chest should be observed for symmetrical expansion and the anesthesiologist should confirm placement of the tube with carbon dioxide return. The skin around the tracheostomy is usually not closed but the wound is packed with gauze. A chest X-ray is always ordered after a tracheostomy.

Figure 1 showing a tracheostomy tube with stylet. Image from
http://en.wikipedia.org/wiki/Tracheotomy#mediaviewer/File:Tracheostomy_tube.jpg
Selection of Tracheostomy Tube
In general, it is recommended that the smallest size tube be selected that just fits into the trachea. The guiding rule of thumb is that the tube should occupy 80% of the tracheal diameter. For an averaged size female, a size 6 Shiley-cuffed tracheostomy tube and in men a size 7/8 is appropriate. It is best to avoid large tubes because they can be difficult to insert and can lead to damage to the tissues. If the tracheostomy is being done in a patient with thick secretions, then a size 7/8 tube is recommended. The tube size if often difficult to assess in patients who are obese or have a short neck. If a short tube is selected, then it will press against the posterior tracheal wall. Over time this can result in obstruction and delayed ulcer formation. A tracheal tube that is too long will have a tendency to curve anteriorly and may erode through the anterior tracheal wall. It is well known that long tracheal tubes can erode into the innominate artery.
In adults, cuffed tracheal tubes are used as they allow for positive pressure ventilation. They may even prevent aspiration. However, presence of a cuff can cause irritation of the mucosa and trap secretions. All cuffed tubes need to be deflated regularly at intervals of 4-6 hours to prevent pressure necrosis on the tracheal wall.
Postoperative Details
After the tracheostomy is completed, the patient is usually taken back to the ICU. The real work now starts with ensuring that the patient is ventilating and oxygenating without difficulty. During the first few days, the patient must be closely monitored to avoid complications like bleeding and dislodgement of the tracheostomy tube. In most new tracheostomies, the amount of secretions are increased and hence frequent pulmonary toilet is required. Unfortunately, excess suctioning can also lead to tracheal ulcerations so one has to be gently during the process. Further the suctioning should be limited to the length of the tube and for no more than a few seconds at a time. Excess suctioning can lead to removal of oxygen from the airway and can quickly lead to hypoxia. To prevent development of thick viscous secretions, the ventilated oxygen must be humidified. Mucus plugs can quickly form in the presence of thick secretions and cause life-threatening blockages.
As a rule, the original tracheal tube should be left in the airways for at least seven to twelve days to allow a tract to form. The sutures holding the tracheostomy tube can then be remove. This also allows for better cleaning of the stomal and neck area. If the reason for a tracheostomy was due to an acute obstruction in the upper airway and no lung disease, then weaning can be attempted by downsizing the tracheostomy tube immediately. Every shift the nurse or the respiratory therapist should ensure that the skin and stoma site are clean- this is to ensure skin organism from colonizing on the raw stomal surface.
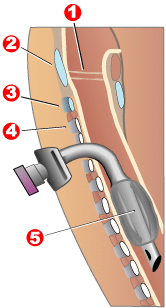
Figure 2 shows placement of a tracheostomy tube. Legends 1= vocal cords, 2 is cricoid cartilage, 3 is first tracheal ring, 4 is second tracheal ring and 5 is a cuffed tracheal tube. Image from
http://en.wikipedia.org/wiki/Tracheotomy#mediaviewer/File:Tracheostomy_tube.jpg
Within a few weeks, most patients on a tracheostomy become less agitated and are ready to wean. At this time the balloon cuff can be deflated periodically and the patient should be encouraged to close the stoma with the fingers and try speaking and or coughing.
After a tracheostomy, consultation with a speech therapist is recommended. These professionals can help assess the swallowing capability. As the patient starts to speak, this also allows reestablishment of the normal airflow down the pharynx and trachea and there is less reliance on the tracheostomy.
Today there are several one-way valve devices that open during inspiration but close during speech. Although much is made of fenestrated tracheostomies, the physician can simply deflate the original tube or downsize to get the same benefit. As the patient tolerates speaking, the tracheostomy can be plugged. The patient must be taught to remove the plug in case he or she develops hypoxia. Patients with obstructive sleep apnea should be instructed to keep their tubes plugged during the day.
A speech therapy consult will also evaluate the ability of a patient with a tracheostomy to swallow. Swallowing is always difficult initially but some type of oral intake is possible after four to six weeks. The risk of aspiration must be evaluated prior to any feeding. Because many patients go home with a tracheostomy, family education is vital. The tracheostomy nurse can provide details on the equipment needed and all family members should feel comfortable with the equipment before the patient is discharged.
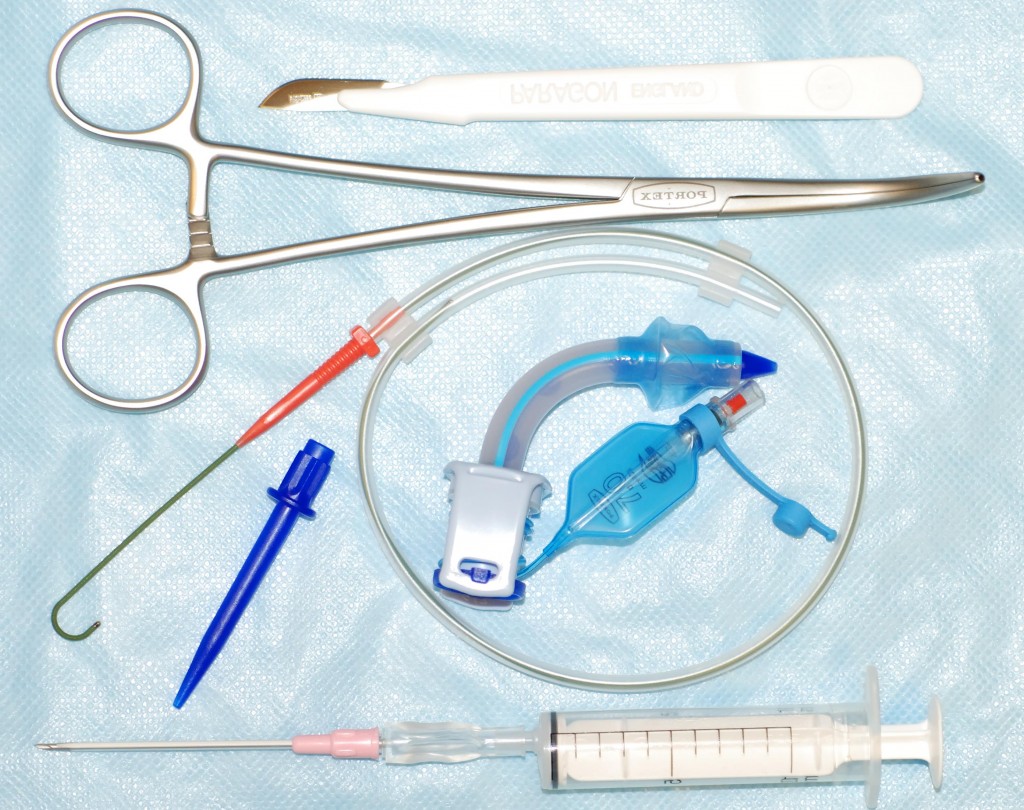
Figure 3 shows a percutaneous tracheostomy set. This set is sometimes used to perform a tracheostomy at the bedside.
Immediate Complications
Tracheostomy can present with immediate complications if the procedure is done hurriedly or by junior staff. One of the most common complications seen immediately after a tracheostomy is loss of respiratory drive. This may occur in a conscious patient and thus he or she must always be transported back to the floor or ICU on a ventilator and be gradually weaned.
Bleeding is a very common complication of tracheostomy. If the surgeon has deviated from the midline or failed to ligate the thyroid vessels, torrential bleeding can occur. When performing the tracheostomy, attention must be paid to cut edges and vessels.
In children, pneumothorax can occur from direct injury to the lung apex when the dissection is deep in the neck. High inspiratory pressures or an agitated child can increase the risk of pneumothorax.
In rare cases, the surgeon dissects laterally and causes injury to one or both laryngeal nerves. This can be catastrophic and results in a permanent tracheostomy.
Finally, most surgeons open the trachea with a knife. Use of cautery to incise cartilage can lead to combustion and fire because of the presence of oxygen.
Early Complications
Bleeding. Early bleeding is a very common complication of a tracheostomy. Despite excellent hemostasis, blood may sometimes soak the gauze overlying the tracheostomy tube. This is often due to increased blood pressure, which occurs when the patient awakens from anesthesia. Moreover, sudden coughing episodes also contribute to the bleeding. This bleeding is usually controlled by lowering blood pressure and packing the wound with gauze. If the packing remains in the tissues for more than 24 hours, prophylactic antibiotic administration is necessary. If the bleeding is continuous, then a return to the OR is mandatory. Sometimes a blood vessel may have slipped a ligature or was not properly cauterized.
In some cases, an ill-fitting tube or overzealous suctioning of the tracheal secretions can lead to bleeding. This is usually due to irritation or ulceration of the skin near the trachea.
Mucus plugs. One very common complication of a tracheostomy is plugging or obstruction with mucus plugs. This complication can be decreased with use of dual cannula tubes. The inner cannula can be removed on a regular basis for cleaning, while the outer tube maintains the patency of the newly created tract. However, any time a patient develops respiratory distress, a mucus plug should be suspected immediately. Anyone with thick, viscous secretions should be frequently suctioned to prevent clogging of the tube.
Tracheal inflammation occurs in all patients following a tracheostomy. The causes may be an ill-fitting tube, frequent suctioning or excessive patient movement with a rigid tube in the neck. One way to prevent this is to humidify all oxygen entering the airways. Second, the tracheal tube circuit should be established to prevent excessive motion on the tissues and prevent ulcerations.
In some cases, the tracheal tube may become displaced and may need changing. However, this can be dangerous if the patient has a fresh tracheostomy; an anesthesiologist should be on standby. An Ambu bag and preparations for oral intubation must be available prior to any change of a fresh tracheostomy tube. Some doctors change the tracheal tube over a nasogastric tube for safety. In some cases, fiberoptic laryngoscopy may be used to introduce the tracheotomy tube under direct visualization. However, if the tracheal tract becomes lost, do not hesitate to orally intubate the patient. Misplacement of the tracheal tube in the mediastinal space or subcutaneous space is not rare. This may present as subcutaneous air or a pneumothorax.
Subcutaneous emphysema. This is a common occurrence when using a large tracheal tube with no room for air to escape. Occasionally this excess air may present as subcutaneous emphysema or a pneumothorax. The best way to treat this complication is to loosen the collar and use a small tracheal tube.
For pneumothorax, a chest tube may be needed. Any time there is a malfunction of a tracheal tube, a chest X-ray is highly recommended.
Bacterial colonization. Colonization of the trachea with bacterial flora is inevitable. However, proper wound care and tracheal hygiene will prevent the development of frank cellulitis. If a long tracheal tube is used, atelectasis of the left lobe can result. After viewing the chest X-ray, a shorter tube should be used.
Late Complications of Tracheostomy
Bleeding is the most common complication and can occur for many reasons. If the tracheostomy tube inserted is placed too deep in the trachea, it can abut against the anterior tracheal wall and result in a tracheoinnominate artery. Many of these patients will present with episodic bright red blood coming out of the trachea. The initial bleed may be a herald small bleed but can be very frightening. At least 0.6% of tracheostomies are associated with this complication and urgent surgery can be life saving. Even with prompt surgery, the mortality rates are very high. If one suspects a tracheoinnominate artery fistula due to the sentinel bleed, an urgent thoracic surgery consult should be made. Sometimes a bronchoscopy can be performed to determine the site of bleeding but often the blood in the trachea obscures any visibility. In rare cases, one may be able to see the site where the tracheostomy tube has eroded through the wall. When a tracheoinnominate artery fistula is suspected, the tracheostomy tube should be removed and replaced with a slightly larger endotracheal tube. The balloon in the endotracheal tube should be inflated as this can tamponade the blood vessel and protect the airway. If the balloon fails to tamponade the bleeding, the therapist or the doctor should quickly insert a finger behind the sternum and press on the back of the chest wall. In the meantime, a call should be made to the thoracic surgeon and operating room. No time should be wasted transporting the patient to the operating room.
In some cases, the mild to moderate bleeding may occur due to the granulation tissue at the tip of the tracheostomy tube. These granulations are easily visualized by performing a laryngoscopy. The site should be cauterized and packed with some type of gauze. Today, we also have glues that can cover up the area and minimize the bleeding. In any cases, cauterization of granulation tissue is best performed in the operating room where there is good lighting and support staff if needed.
If the tracheal tube is not fitted properly, it can lead to softening of the tracheal wall. The resulting weakening also known as tracheomalacia may present with stridor during inspiration. This condition is diagnosed with fluoroscopy or laryngoscopy.
Stenosis is a frequent problem when the tracheostomy is done in the first trachea ring. The laryngeal stenosis that results can be very difficult to resolve. Stenosis can also occur at the site of the tracheostomy from prolonged irritation by the cuff. The exact incidence of post-tracheostomy stenosis is not known because many patients either are not investigated or are not symptomatic. With the advent of high-volume low-pressure cuffs, the incidence of stenosis has significantly declined. In any case, it is vital that the cuff never be overinflated. Periodic deflation of the cuff is necessary on a regular basis. Tracheal stenosis usually does not develop immediately but may take several weeks or months to manifest. Often the diagnosis is delayed because the symptoms are mistaken for bronchitis or mucus plugs. The treatment for symptoms of tracheal stenosis is surgical revision. However, with advances in percutaneous technology, stenting has now become a viable option for many people with tracheal stenosis.
A rare complication of prolonged tracheostomy is a tracheoesophageal fistula. This often occurs when the patient has a rigid nasogastric tube and an overinflated tracheostomy tube. The rubbing of these the two devices leads to erosion of the posterior tracheal wall into the esophagus. The condition often presents with food particles coming out of the trachea. A diagnosis is made by bronchoscopy and/or a barium swallow. The only treatment for this condition is surgery. The trachea and esophagus are separated and a muscle flap is usually interposed between them. Stenting of the esophagus or trachea is also an option. The patient may require a jejunostomy tube while the tissues are healing.
Prolonged intubation can cause a tracheocutaneous fistula, which is a non-healing fistula. Treatment usually involves excision of granulation tissue and a layer closure. If the tracheocutaneous fistula persists, the physician should rule out a distal obstruction via laryngoscopy.
Granulation tissue build-up is very common at the stoma site and can lead to occasional bleeding. The bleeding can be cauterized with silver nitrate. Untreated granulation tissue can lead to fibrosis and stenosis.
In some patients there may be difficulty cannulating. The trachea stoma may be obstructed, there may be fractured cartilage, or the patient may be very anxious. Such cases should be evaluated with laryngoscopy.
Sleep Apnea
Some surgeons do recommend a tracheostomy in patients with sleep apnea. However, this is a controversial topic and not universally accepted. In the past, the standard procedure for sleep apnea patients was a tracheostomy. However, today there are other options for treatment of sleep apnea like CPAP and uvulopalatopharyngoplasty. Tracheostomy is last resort treatment when all else fails. Today there are several technical surgical modifications that have been developed to create a permanent tracheostomy in sleep apnea patients. This includes creation of skin flaps, tapping the chest-down and chin-up position. Unfortunately, these patient positions are not always well tolerated.
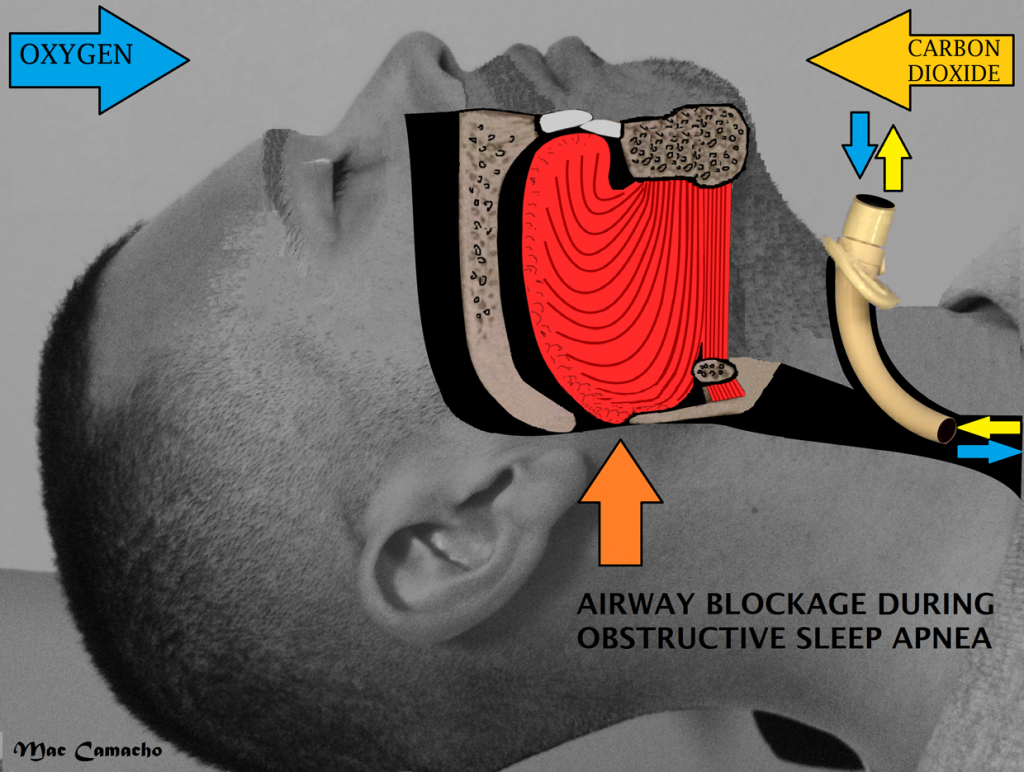
Figure 4 showing position of tracheostomy tube in a supine patient. Image courtesy
http://en.wikipedia.org/wiki/Tracheotomy#mediaviewer/File:Tracheostomy_tube.jpg
Children
The reason for a tracheostomy in children is done primarily for the same reasons as adults. However, in children most physicians tend to wait a little longer while on the oral tracheal tube before ordering the procedure the reason is that children often abruptly turn around and are a little easier to wean off the orotracheal tube. In children, the most common reason for a tracheostomy is airway obstruction, followed by respiratory failure from ARDs and need for aggressive pulmonary toilet. Unlike the adult, tracheostomy in a child has to be done with great care. On either side of the trachea, the surgeon will place strong stay sutures at the time of surgery. The reason for this is that children have a short neck and often the tracheotomy tube can easily dislodge, this can immediately become life threatening. Hence, pulling on the sutures brings the trachea anterior to the stoma and another cannula can quickly be inserted under vision.
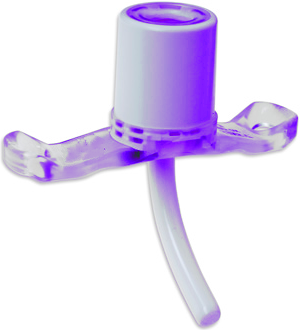
Figure 5 shows an uncuffed tracheostomy tube for use in children.
Further too much dissection in and around the trachea in children is avoided because of the potential for injury. Even with this awareness, complications of tracheostomy in children continue to occur and are often associated with high mortality. Thus, a tracheostomy in a child should not be taken lightly as the potential for complications is high. Unlike adults, children do not tolerate hypoxia well.
Tracheostomy Weaning
In most cases of temporary tracheostomy, the weaning starts after the patient has recovered from his/her original illness. The weaning process is slow and gradual. Once the patient is able to follow commands and has recovered, the decision to decannulate begins by downsizing the original cannula. This allows the patient to start breathing through the mouth. Decannulation is a slow process and should not be rushed. The patient should be allowed to slowly tolerate plugging of the tracheostomy tube during the waking hours as long as he/she doesn’t develop oxygen desaturation of respiratory difficult.

Figure 7 shows a patient weaned off a tracheostomy tube.
Tracheostomy can be life saving and has significantly less morbidity than an oral endotracheal tube. Tracheostomy can be used indefinitely in most patients.
When the patient is able to tolerate decannulation during the daytime, the stoma is closed with a plug or tape. The patient is then taught how to occlude the stoma hole with his/her fingers and start to speak. This maneuver also allows the patient to cough up any secretions in the oral cavity. Once the cannula is removed, it quickly narrows and then closed in a few weeks. However, the skin close may takes months or longer to close. Most people do develop a prominent scar after a tracheostomy. Respiratory therapists can help lower the morbidity of a tracheostomy by paying attention to the airway secretions and encouraging coughing.
References
- Durbin CG Jr. Tracheostomy: why, when, and how? Respir Care. 2010;55(8):1056-1068.
- Liu CC, Livingstone D, Dixon E, Dort JC. Early versus Late Tracheostomy: A Systematic Review and Meta-Analysis. Otolaryngol Head Neck Surg. 2015;152(2):219-227
- Meininger D, Walcher F, Byhahn C. Tracheostomy in intensive care long-term ventilation: indications, techniques and complications. German Chirurg. 2011;82(2):107-110,112-115.
- Lissauer ME. Benefit, timing, and technique of tracheostomy. Curr Probl Surg. 2013;50(10):494-499.
- Higginson R, Jones B, Davies K. Airway management for nurses: emergency assessment and care. Br J Nurs. 2010;19(16):1006-1014.

