
Diaphragmatic Paralysis 2.0 CE Hours
Course Objectives:
- Describe the anatomy of the diaphragm.
- List causes of diaphragmatic paralysis.
- List the signs and symptoms of diaphragmatic paralysis
- Discuss the diagnosis and work up of a patient with diaphragmatic paralysis
- Describe the treatments for diaphragmatic paralysis
Abstract
Diaphragmatic paralysis can be unilateral or bilateral. Even though the diaphragm is the major muscle of respiration, there are other respiratory muscles, known as accessory muscles that also play a role in respiration. These include the scalene, parasternal portion of the internal and external intercostal muscles, sternocleidomastoid, and trapezius. In patients with bilateral diaphragmatic paralysis, these accessory muscles adapt and assume some of the work of breathing by contracting more strongly. However, the accessory muscles do not have the reserve capacity of the diaphragm and when they tire out, the patient will develop respiratory failure. Unilateral diaphragmatic paralysis generally has a better prognosis.
The diaphragm is a very important muscle for ventilation. During inspiration, it creates negative intrathoracic pressure, which initiates ventilation. The phrenic nerve originates from cervical neurons C3-C5 and provides both sensory and motor function to the diaphragm. When the diaphragm contracts, the cone shaped muscle lowers intrapleural pressure during inspiration, expands the rib cage and the negative pressure created in the chest cavity results in movement of air into the lungs. Diaphragmatic paralysis may be unilateral or bilateral and be a cause of dyspnea. Injury to the phrenic nerve is the most common cause of diaphragmatic paralysis. When the diaphragm is paralyzed, the body is able to adapt to some degree by using other muscles of respiration.
Function of the diaphragm
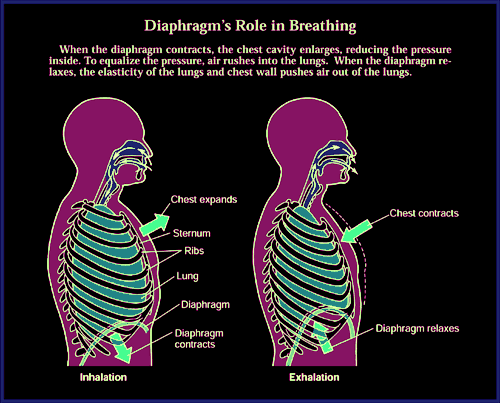
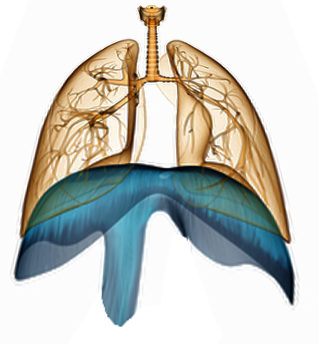
The diaphragm is a large dome shaped muscle that separates the abdomen from the chest cavity. The superior surface of the diaphragm from the floor of the chest cavity and the inferior surface from the roof of the abdominal cavity. The diaphragm is a major muscle involved in respiration. It separates the chest from the abdominal cavity and is responsible for creating the negative pressure in the chest cavity during inspiration. The displacement of diaphragm into the abdomen during inspiration results in expansion of the chest and creation of negative pleural pressure, which then results in air flowing into the airway and lungs.
Figure 1 showing relationship of lungs, heart and diaphragm.
 Anatomy of diaphragm
Anatomy of diaphragm
The diaphragm, the most important muscle of inspiration, is one confluent uninterrupted structure, composed of a central tendon, surrounded by muscle fibers. The dome shaped diaphragm also has many peripheral attachments which ensure that the muscle remains fixed during contraction. The peripheral attachments to the front insert at the xiphoid and laterally along the costal margin and ribs. Along the back, the muscle fibers insert into the vertebra at T12, the right and left crus, and lumbar vertebrae L1 and L2. The diaphragm has three major openings, which allow structures from the abdomen to enter the chest cavity. These structures include passage of the aorta, the esophagus and vena cava.
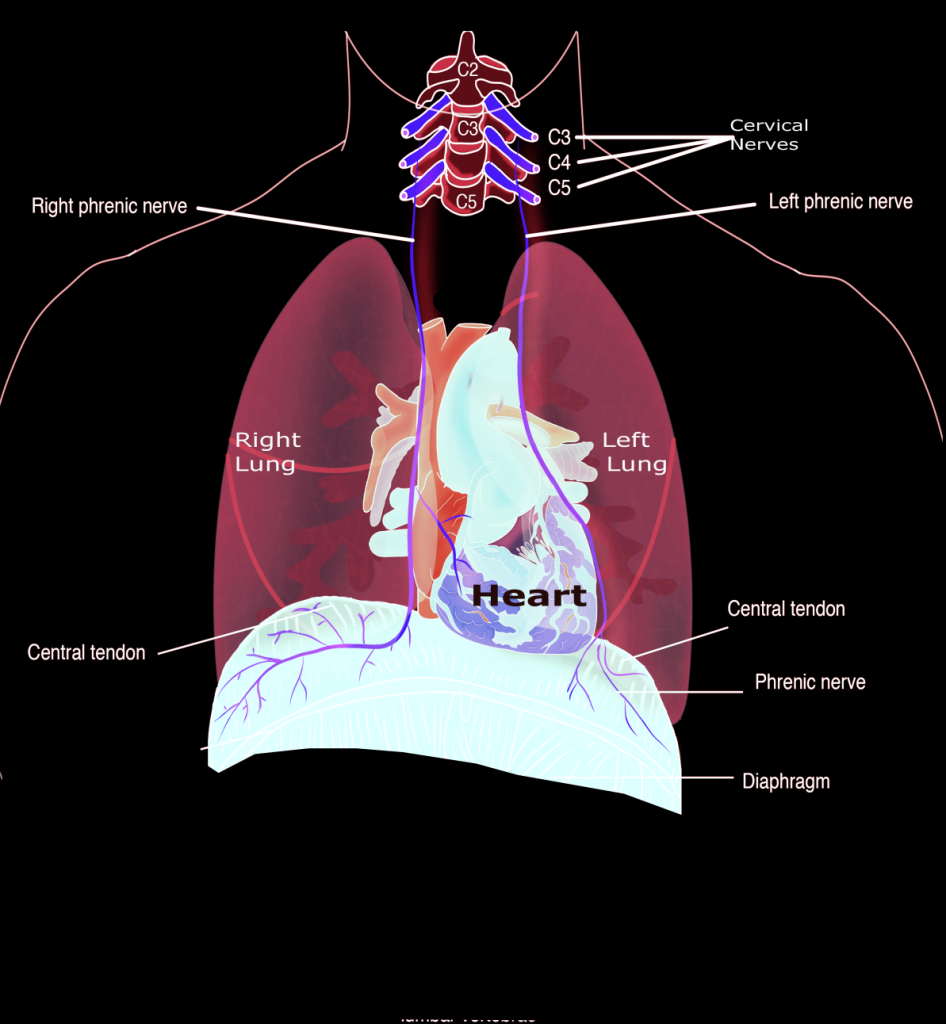
The diaphragm is primarily innervated by the phrenic nerve that is formed from the fusion of neurons from C3, C4 and C5. The major function of the diaphragm is to assist in breathing during inspiration. When stimulated, the diaphragm contracts and moves inferiorly, thus creating an increased volume in the chest cavity and a negative pleural pressure. The reduced intra thoracic pressure then passively encourages air to pass from the nose into the airways. When the diaphragm relaxes it pushes upwards and the air is exhaled because of the elastic recoil of the lung tissues and lining of the thoracic cavity. The diaphragm also has non-respiratory functions such as assisting in vomiting, defecation and passage of urine by generating increased abdominal pressure. The diaphragm also prevents acid reflux by exerting external pressure on the esophagus and acting as a one-way valve.
Figure 2 shows normal physiology of breathing and diaphragmatic contraction,
Course of Phrenic Nerve
The phrenic nerve originates in the cervical neck between C3-C5 and then takes a vertical pathway into the chest. It courses behind the sternocleidomastoid muscle, between the subclavian vessels and then enters the apex of the chest. The left phrenic nerve runs adjacent to the thoracic duct, crosses anterior to the internal mammary arteries and passes in front of the aortic arch and main pulmonary artery. It then courses anterior to the pericardium. The right phrenic nerve follows the superior vena cava and runs alongside the right pericardium, eventually piercing the diaphragm lateral to the vena cava hiatus. The left phrenic nerve pierces just lateral to the left ventricle border. Each nerve divides on the surface of the diaphragm into four branches.
Figure 3 showing course of phrenic nerve from the neck to the diaphragm.
Pathophysiology
Diaphragmatic paralysis can be unilateral or bilateral. Even though the diaphragm is the major muscle of respiration, there are other respiratory muscles, known as accessory muscles that also play a role in respiration. These include the scalene, parasternal portion of the internal and external intercostal muscles, sternocleidomastoid, and trapezius. In patients with bilateral diaphragmatic paralysis, these accessory muscles adapt and assume some of the work of breathing by contracting more strongly. However, the accessory muscles do not have the reserve capacity of the diaphragm and when they tire out, the patient will develop respiratory failure.
Epidemiology
The exact incidence of diaphragmatic paralysis is not known because the disorder is often not reported or the diagnosis is missed. In any case, the numbers are underreported. Unilateral diaphragmatic paralysis is often asymptomatic and symptoms depend on underlying lung disease. In most cases unilateral diaphragmatic paralysis is incidentally discovered during imaging studies. Overall, the left hemidiaphragm is more likely to be paralyzed than the right side. The patients who do tend to develop symptoms are those who have underlying lung disease. Bilateral diaphragmatic paralysis is not common. Diaphragmatic paralysis is more common in males than females. The disorder can occur at any age.
Causes
Unilateral diaphragmatic paralysis
Malignancy is the most common cause of unilateral diaphragmatic paralysis. About 30% of patients with centrally located lung tumors will develop some degree of diaphragmatic paralysis; the centrally located tumors often invade the phrenic nerve that results in diaphragmatic paralysis. However, in people with no lung malignancy no cause is ever found. Other rare causes of unilateral diaphragmatic paralysis include the following:
- Blunt cervical trauma
- Cervical spondylosis
- Herpes zoster
- Surgical trauma (mainly thoracic)
- Supraclavicular brachial plexus block. This can sometimes be avoided by the use of ultrasound to assess needle placement)
- Upper cervical radiculopathy as a cause of unilateral diaphragmatic paralysis has also been reported.
Bilateral diaphragmatic paralysis
The most common causes are systemic neuromuscular disorders like post-polio syndrome and amyotrophic lateral sclerosis. Other rare causes of bilateral diaphragmatic paralysis include the following
- Guillain-Barre syndrome
- Muscular dystrophy (acid maltase deficiency),
- Myopathies
- Parsonage-Turner syndrome (neuropathy of brachial plexus)
- Thoracic trauma (including open heart surgery)
Diaphragmatic dysfunction following cardiac surgery
Phrenic nerve injury is sometimes seen during open heart surgery and there are several reasons for it which include the following:
- The phrenic nerve injury may occur following use of cold cardioplegic solutions or it may be related to mechanical stretching of the nerve during placement of the sternal retractor. The incidence of phrenic nerve injury with the use of warm cardioplegia remains unknown.
- Another common reason for phrenic nerve injury is during harvesting of the internal mammary artery for coronary artery bypass. The harvesting of the internal mammary requires the use of a retractor and there is more traction place in the apex of the chest where the phrenic nerve runs. Not only does this result in phrenic nerve injury, the retractor can lead to fracture of the sternum, ribs and lead to more pain in postoperative period. Dissection of the IMA can also lead to decrease supply to the ipsilateral intercostal muscles and induce mechanical injury to the phrenic nerve.
The exact number of individuals who develop phrenic nerve injury following open-heart surgery is unknown but the numbers are not miniscule. The patient may present with an elevated left hemidiaphragm, which is often mistaken for pneumonia, left pleural effusion or atelectasis. Symptoms of left phrenic nerve injury following open-heart surgery also depend on underlying lung function and other patient comorbidities.
When left phrenic nerve injury is diagnosed after open heart surgery, conservative treatment include chest physical therapy, treatment of any underlying lung condition like COPD, asthma, prevention and treatment of pneumonia, and ambulation with deep breathing is recommended. In adults with unilateral diaphragmatic paralysis, diaphragmatic plication is rarely needed. Children on the other hand, especially infants, may need diaphragmatic plication to help them wean off the ventilator.
Clinical Presentation
Patients with diaphragmatic paralysis may experience a wide range of symptoms: from being asymptomatic, symptomatic only with exercise, or develop progressive respiratory insufficiency and require permanent mechanical ventilation. Symptoms depend on the preexisting cardiopulmonary status, the extent of paralysis (unilateral or bilateral) and on the nature of the paralysis (acute or chronic). Some symptoms are distinct and should always raise the diagnosis of diaphragmatic paralysis.
Diaphragmatic paralysis is known to be associated with decreased vital capacity at rest, which is more severe in the supine position. The accessory muscles of ventilation need to work a lot harder and there is usually derangement in gas exchange due to mismatched ventilation to perfusion in the affected areas of the lung. This will show up as hypoxemia at rest, which is more obvious during sleep and exercise. Therefore individuals may be asymptomatic at rest or in the erect position. Thus, it is important to ask pertinent questions regarding orthopnea.
The majority of cases of unilateral diaphragmatic paralysis are discovered incidentally after undergoing a chest x-ray for the work up of another disorder. Most patients have no symptoms at rest, whereas some may experience shortness of breath upon exertion. Over time, patients with unilateral diaphragmatic paralysis develop a decrease in exercise endurance. Patients with underlying lung disease and unilateral diaphragmatic paralysis will often have symptoms at rest. Orthopnea may also be present in some of the patients, but it is much less in intensity compared to patients with bilateral diaphragmatic paralysis.
The majority of patients with bilateral diagrammatic paralysis are symptomatic. The symptoms are often severe in the presence of underlying lung disease. In patients with bilateral diaphragmatic paralysis, other symptoms may include confusion, morning headaches, and signs of cor pulmonale. Chest examination usually reveals limitation of diaphragmatic excursions, absent breath sounds and bilateral lower chest dullness. Patients are usually tachypneic and may use accessory respiration muscles. The diagnostic finding is a paradoxical inward movement of the abdomen with inspiration.
In addition, in the presence of any underlying lung pathology, these patients often need immediate mechanical ventilation.
In some patients with bilateral diaphragmatic paralysis, the complaint may be vague abdominal pain which is due to the excessive strain on the abdominal muscles. Most patients develop shallow breathing, tachypnea and the patient usually adopts the recumbent position. These patients may have impaired gas exchange even in the presence of mild lung disease. Respiratory difficulties, hypoxia and hypercarbia are common features. In some patients, night sweats have also been reported. Often the symptoms are severe when lying supine and the disorder is often confused with congestive heart failure.
Other symptoms that may be associated with diaphragmatic paralysis include anxiety, diaphoresis, insomnia, excessive daytime somnolence, morning headache and fatigue. In some patients, nonspecific GI symptoms may include nausea, heartburn, regurgitation and upper abdominal or chest pain.
Acute paralysis of the diaphragm
The majority of patients who suddenly develop acute diaphragmatic paralysis will develop symptoms. This is chiefly because they have always been using both diaphragms to breathe and now with paralysis on one side, the body is not suddenly able to adapt. The patient may acutely feel chest heaviness, dyspnea, shoulder pain and severe orthopnea. However, with time, the symptoms diminish as the accessory muscles gradually adapt to the loss of the diaphragms. In some cases, the symptoms do subside because the paralysis spontaneously resolves.
There are some people who have developed acute diaphragmatic paralyses after a viral infection, akin to what is seen in bell palsy. The use of antiviral agents like valacyclovir has been useful in some patients.
Physical Exam
The findings on a physical exam depend on whether the patient has unilateral or bilateral diaphragmatic paralysis. In some patients, the key diagnostic feature on a physical exam is paradoxical inward movement of the abdomen with inspiration. This sign is important and easily recognizable if the patient lays supine and is relaxed. Paradoxical movement of the abdominal wall is almost always seen with bilateral paralysis, but common even with unilateral disease. Occasionally, no paradoxical movement of the abdominal wall, but limited or asymmetrical excursion of the affected side abdominal wall can be seen. However, paradoxical movement of the abdominal wall is occasionally present in healthy subjects, especially if not relaxed during the examination.
On palpation of the chest just underneath the costal margin, the healthcare provider may be able to feel the descent of the hemidiaphragm during inspiration.
Auscultation may reveal dullness to percussion and absent breath sounds over the lower segments of the chest on the involved side. Excursion of the involved hemithorax is often decreased compared to the unaffected side. In patients with bilateral diaphragmatic paralysis one may notice tachypnea and use of accessory respiratory muscles.
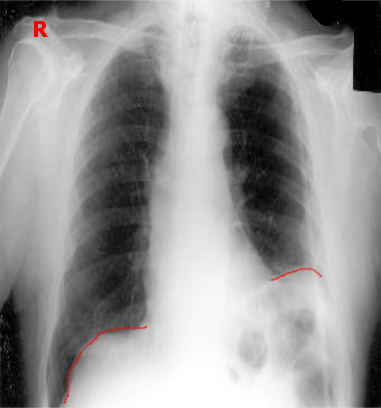
Figure 4 showing bilateral diaphragmatic paralysis. The diaphragm becomes floppy and moves inside the chest.
Differential Diagnosis
The symptoms of diaphragmatic paralysis are not clear and the disorder can be confused with pneumonia, pleural effusion, pulmonary embolism or congestive heart failure. Other disorders that may be confused with diaphragmatic paralysis include eventration of the diaphragm, which is congenital. Thus, it is important to rule out the other causes during the work up.
Diagnosis
The diagnosis and work up of diaphragmatic paralysis follows an algorithm based on symptoms and degree of suspicion. Based on the history and physical presence of paradoxical movement of the abdominal wall, may be the first clue that the patient has diaphragmatic paralysis. One may first obtain laboratory studies followed by imaging tests.
Laboratory Studies
An arterial blood gas is usually the one laboratory study that is needed to assess ventilation and hypoxemia. Hypoxemia may be due to the atelectasis and the ventilation perfusion mismatch. In people who have progressive disease, the hypoxemia often progresses. Hence, an arterial blood gas can also be used to follow up patients with diaphragmatic paralysis. As the patient tires the arterial blood gas will start to show progressive hypercapnia.
Diaphragmatic paralysis may be an early feature of a systemic disorder like myopathy, or of motor neuron disease, all of which require evaluation. If hypothyroidism is suspected, thyroid function and muscle enzymes should be ordered.
Imaging Studies
Chest X-ray
The first suspicion of diaphragmatic paralysis is usually asymmetric elevation of the hemidiaphragm on a plain chest x-ray. The X-ray may also show patchy atelectasis above the diaphragm, and small lung volume. Bilateral paralysis of the diaphragm is more difficult to recognize, as there is no asymmetry.
Chest X-ray showing an elevated left hemidiaphragm.
Sniff test
When diaphragmatic paralysis is suspected on a chest x-ray, it can be confirmed by the sniff test using fluoroscopy or ultrasound. During the sniff test, the paradoxical movement of the paralyzed diaphragm occurs upwards with inspiration; in contrast the unaffected muscle moves downwards. The movement of the diaphragm can be visualized with ultrasound or fluoroscopy. An important observation on ultrasound is that the diaphragmatic muscle will not thicken during contraction.
Fluoroscopy
On fluoroscopy one may see the diaphragm move paradoxically upwards on inspiration. Unfortunately, the sniff test is not very specific because close to 6% of normal individuals also exhibit paradoxical motion on fluoroscopy. In addition due to compensatory use of accessory respiratory muscles, apparently normal decent of the diaphragm may also be seen with sniff test in bilateral diaphragmatic paralysis.
Ultrasound
Ultrasound is a portable and a relatively simple test for diagnosing paralysis of the diaphragm in the adult population. The test can be performed at the bedside. The paralyzed side will show no active movement of the diaphragm downwards during inspiration and abnormal paradoxical movement (i.e., cranial movement on inspiration), particularly with the sniff test. Ultrasound can also be used to assess the thickness of the diaphragm during inspiration. If no thickness is observed during inspiration, this is a sensitive test for diaphragmatic paralysis. Ultrasonography can also be used to serially monitor patients with diaphragmatic paralysis for recovery.
Additional studies
The studies described above are usually sufficient to establish the diagnosis of diaphragmatic paralysis or of severe diaphragmatic dysfunction. However, in some cases more specific measures are needed.
Lung Function
Pulmonary functions tests are now routinely done in patients with diaphragmatic paralysis to monitor progression of disease. The vital capacity is measured in the supine and upright position and is the most important test. Because diaphragmatic paralysis decreases lung compliance, the testing will also reveal a restrictive pattern. Normally in recumbent individual vital capacity decreases by 10%, however, in patients with bilateral diaphragmatic paralysis, there will be a 50% decrease in vital capacity when supine. This drop in vital capacity is due to cephalad displacement of the abdominal organs into the chest. Oxygen saturation often falls markedly during sleep (chiefly during rapid eye movement phase) and with exercise. Diffusion capacity may be near normal in diaphragmatic paralysis and if markedly abnormal, it justifies a search for an alternative cause.
The problem with pulmonary function testing in patients with diaphragmatic paralysis is that the testing is not always reliable or consistent; the test is very observer dependent and often the results cannot be reproduced. In addition, there is no correlation between symptoms and degree of diaphragmatic paralysis
EMG
The EMG response of the diaphragm can be measured at the muscle insertion along the intercostals spaces with surface electrodes. The stimulation can be done with or without phrenic nerve stimulation. The study allows one to monitor signals and nerve conduction velocities can be determined. The test may help differentiate myopathic from neuropathic causes of diaphragmatic paralysis. However, the technique is not easy and fraught with errors. The electrical leads can often detect signals from other nerves and there is often a lot of background noise that makes interpretation of data difficult. Plus, because of the depth of subcutaneous tissue in individual, the depth of needle placement in the body is also is variable.
Measurement of transdiaphragmatic pressure
This is the criterion standard for diagnosis of diaphragmatic paralysis. This test is performed by placing a thin-walled balloon transnasally at the lower end of the esophagus, which allows one to measure changes in pleural pressure. Then, a second balloon manometer is placed in the stomach to monitor alterations in intra-abdominal pressure. In normal circumstances, gastric pressure increases during inspiration, whereas esophageal pressure decreases or becomes more negative during inspiration, revealing an increased gradient during normal inspiration. In individuals where the sniff test is unrevealing but suspicion for diaphragmatic paralysis is still high, transdiaphragmatic pressure should be considered. However, one should utilize the assistance of a pulmonologist and gastroenterologist to interpret the results. This test may of help in differentiating diaphragmatic paralysis from other causes of respiratory failure. Unfortunately, the test is not standardized and there is a great variation in even normal pressure measurements.
CT Scan and MRI
Even though most cases of diaphragmatic paralysis are idiopathic, in up to 5-30% of patients a thoracic malignancy is present. Therefore, when the cause is not obvious, CT scanning or MRI is recommended. MRI can also reveal the extent of nerve involvement and location of the problem.
Management
Treatment options
Most patients with unilateral diaphragmatic paralysis need no specific therapy. If an underlying cause of the paralyses is discovered, then one should try and reverse it. Symptomatic patients or those with preexisting lung disease especially if marked orthopnea exists may benefit from non-invasive nocturnal ventilatory support. This mode of therapy may offer improvement in sleep quality, daytime functioning and improvement in arterial blood gas.
Even in patients in whom the etiology is unknown, supportive care should be offered as in many instances the disorder will gradually reverse spontaneously. This may take a few months or even a year. In the few patients with unilateral diaphragmatic paralysis who are symptomatic with severe dyspnea, surgical plication of the diaphragm may be helpful.
The rationale for anti-viral therapy in patient with acute onset diaphragmatic paralysis following a "viral" prodromal may be treated with antiviral medications.
Diaphragmatic Plication
Diaphragm plication is a very old technique used to tighten up the muscle. The paralyzed diaphragm usually becomes floppy and hence it is plicated or folded on itself to increase the tightness. This reduces the compliance and prevents the diaphragm from moving into the chest during inspiration. The floppy diaphragm is plicated or folded over itself using strong sutures. In selected patients it does provide good results. Plication of the diaphragm prevents the paradoxical motion of the abdominal organs into the chest during inspiration and hence slightly improves ventilation on the affected side. In addition, the procedure also reduces the workload of the normal diaphragm on the other side. Several studies have shown that in selected patients, diaphragmatic plication can improve vital capacity and improve oxygenation by about 10%. In addition, after plication, studies show that some patients do have improved lung function in both supine and erect position. Other studies have shown improvement in symptoms after plication for up to 5 years. However, this degree of improvement in symptoms does not occur in all patients. Most of the data on exercise tolerance and gas exchange following diaphragmatic plication are anecdotal.
Other studies have shown that following diaphragmatic plication, it was possible to wean patients off the mechanical ventilator. Furthermore, the procedure also favors the healthy diaphragm, which now performs less work. Plication of the diaphragm can be done via a thoracotomy or via a thoracoscopic technique. The thoracoscopic approach is less painful, allows faster recovery and has similar results but it is also more expensive.
Diaphragmatic plication is difficult to perform in obese individuals and these patients should first be assessed for a weight loss program. Even when done in obese individuals, the results are not always good. Similarly plication of the diaphragm in patients with neuromuscular disorders does not have benefits and great care should be taken before subjecting them to surgery. The risk of complications is far greater in this patient population.
Phrenic nerve pacing
A relatively new technique for patients with diaphragmatic paralysis is phrenic nerve pacing. The technique has been used to treat patients with upper cervical spinal cord injury and with central respiratory paralyses. For the technique to work, these patients should not have intrinsic lung injury, but must have an intact phrenic nerve. The technique is only used in select centers and is not consistently effective. The benefits do vary. The electrodes are planted around the phrenic nerve in the chest using thoracoscopy. The lead is then attached to a pacemaker. However, before full stimulation, the phrenic nerve must be trained for a few weeks. When effective, phrenic nerve pacing can help the patient regain the ability to be weaned off the ventilator and become ambulatory. It also improves respiratory clearance of mucus and reduces lung infections.
However, prior to phrenic nerve pacing, the integrity of the nerve has to be assessed; the technique is of limited used in patients with atrophy and deconditioning of the diaphragm.
Phrenic nerve pacing has been used to treat cervical quadriplegics but the results are not spectacular. Phrenic nerve pacing is rarely used for isolated unilateral diaphragmatic paralysis. In addition, there are many technical difficulties such as synchronization of other respiratory muscles.
Negative pressure ventilation
The general treatment of bilateral diaphragmatic paralysis depends on the cause and severity. In the past, mechanical ventilation was the only treatment for patients who developed respiratory failure and had severe symptoms. It was soon observed that patients who did not have intrinsic lung disease could be slowly weaned off the ventilator and may be better served with noninvasive ventilation techniques.
Negative-pressure techniques may induce obstruction of the upper airway in patients with diaphragmatic paralysis, especially in those with weak upper airway muscles that unable to counteract the negative pressure generated by the ventilator. Therefore, proper sleep studies are necessary in patients who are being considered for negative-pressure ventilation. Use of positive-pressure ventilation decreases the requirement for screening sleep studies.
Most patients with mild-to-moderate diaphragmatic weakness are able to maintain daytime gas exchange but this may worsen during sleep. Sleep studies and ventilatory-assist device treatments may help identify these patients. Nighttime noninvasive ventilation has been useful in some selected patients with diaphragmatic paralysis. Individuals in whom noninvasive means of ventilation fail to provide benefit may benefit from a rocking bed, pulmonary wrap or positive pressure pneumobelt. There are no good data to show that these technique work.
Tracheostomy with positive-pressure intermittent or permanent ventilation is reserved for patients who are not candidates for less invasive methods or in whom less invasive methods fail.
Nerve reconstruction techniques
Individuals with known phrenic nerve injury may benefit from nerve surgery. The types of nerve procedure that can be used to restore integrity of the phrenic nerve include nerve grafting, neurolysis, and neurotization. These procedures have sometimes been used for unilateral nerve repair in patients who suffered injury as a result of surgery or anesthetic procedures in the neck area.
Endurance and inspiratory muscle training
All individuals with diaphragmatic paralysis are recommended some type of inspiratory muscle training. Daily endurance training has been shown to lead to mild improvement in symptoms of diaphragmatic paralysis.
Course and prognosis
The prognosis of patients with unilateral diaphragmatic paralysis is good as long as they do not have any underlying chronic lung disease. The course only tends to be worse in individuals with underlying lung disease, like COPD or interstitial lung disease. Even those who develop symptoms do improve due to adaptation of the accessory muscles to aid inspiration. Many studies have shown improvement in patient’s months or years after unilateral diaphragmatic paralysis. It is believed by some experts that over time the compliance of the paralyzed diaphragm decreases and thus, there is restricted movement of the diaphragm into the chest with inspiration.
Patients with bilateral diaphragmatic paralysis tend to have a worse prognosis irrespective of the presence of symptoms. Most patients have no exercise endurance and are often short of breath when lying supine. Even those who become ventilator independent continue to struggle and the quality of life is not great. Most patients though require long-term care. Recovery, if it occurs may take years
Conclusion
Diaphragmatic paralysis is a relatively uncommon disorder. In many cases unilateral diaphragmatic paralysis is mild or asymptomatic. The cause in many people is idiopathic. Therefore, it is often undiagnosed or under reported. However, bilateral diaphragmatic paralysis can cause severe symptoms (such as orthopnea and dyspnea which are worse in the supine position and during exercise. Diagnosis in most cases is confirmed by the Sniff test with additional supportive tests such as upright and supine lung function and respiratory muscle forces. These tests are important for follow up. Prompt diagnosis prevents the morbidity of the disorder and early return to daily living activities. In many patients with unilateral diaphragmatic paralysis no specific therapy is needed and in at least 1/3rd of patients the symptoms will improve spontaneously. Symptomatic patients may need nocturnal ventilatory assist and in selected cases diaphragmatic plication or pacing should be considered.
References
- Declerck S, Testelmans D, Nafteux P, et al. Diaphragm plication for unilateral diaphragm paralysis: a case report and review of the literature. Acta Clin Belg. 2013;68(4):311-5.
- Kaufman MR, Elkwood AI, Colicchio AR, et al. Functional restoration of diaphragmatic paralysis: an evaluation of phrenic nerve reconstruction. Ann Thorac Surg. 2014;97(1):260-6.
- Kharma N. Dysfunction of the diaphragm: imaging as a diagnostic tool. Curr Opin Pulm Med. 2013;19(4):394-8.
- Romero FJ, Gambarrutta C, Garcia-Forcada A, et al. Long-term evaluation of phrenic nerve pacing for respiratory failure due to high cervical spinal cord injury. Spinal Cord. 2012;50(12):895-8.
- Shiohama T, Fujii K, Hayashi M, et al. Phrenic nerve palsy associated with birth trauma--case reports and a literature review. Brain Dev. 2013;35(4):363-6.
- Gazala S, Hunt I, Bédard EL Diaphragmatic plication offers functional improvement in dyspnea and better pulmonary function with low morbidity. Interact Cardiovasc Thorac Surg. 2012;15(3):505-8.

