
Comprehensive Disease Management Of Patients With Asthma 3.0 CE Hours
Course Objectives:
- Describe four reasons why asthma is increasing in the U.S.
- Discuss the role of the Respiratory Therapist in treating patients with asthma
- Explain the four components of a comprehensive disease management program for people with asthma
- Discuss the current treatments for people with asthma
- Discuss current research trends in asthma
INTRODUCTION
Asthma is a condition that affects the lungs. Both children and adults can acquire asthma. Some children are born with the condition, while others acquire it later in life. In addition, some adults acquire asthma later in life as well. The Center for Disease Control states that at present the cause and cure for asthma are both unknown, but it can be managed. The primary symptoms of asthma are described as follows:
Asthma causes wheezing, breathlessness, chest tightness, and coughing at night or early in the morning. If you have asthma, you have it all the time, but you will have asthma attacks only when something bothers your lungs[1].
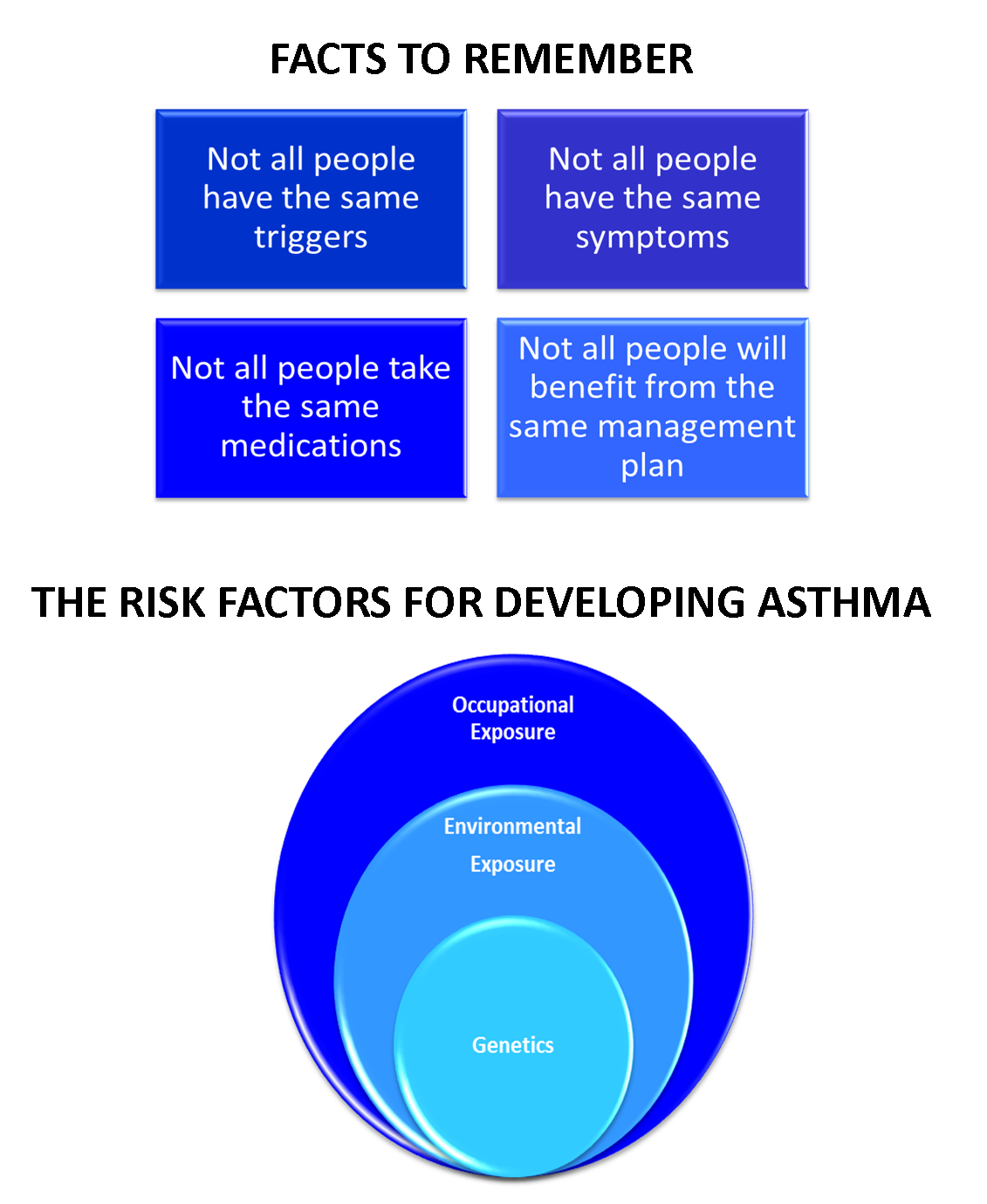
The most common issue with asthma is that it causes breathing ‘attacks’. The lungs become blocked and the person feels as if they are choking. The symptoms listed above are the most common. The primary problem is that less air is coming into the lungs and mucus forms which cause the airways to be even more blocked up. In order to control these symptoms, doctors prescribe an asthma management program which is geared towards the specific individual. In the treatment of people with asthma, it is important for all practitioners to remember that people experience different triggers for their attacks, not all people experience the same symptoms, and not everyone responds to the same treatments (or takes the same medication). Illness is a highly individual experience, and although there will be similarities, some people may experience certain symptoms due to co-morbidity with another condition, or other factors in their life such s extreme stress, obesity, and many others.
POSSIBLE REASONS WHY ASTHMA IS INCREASING IN THE U.S.
The Center for Disease Control is one of the agencies responsible for research into how and why some diseases are on the rise, while others are under control. Researchers have been divided on the facts about asthma. Certainly, environmental factors have been taken into consideration. We all know that pollution is a huge environmental challenge, and some people are more affected by it than others. The reason why this is so is still a research question without an answer. According to the CDC, approximately 1 in 12 Americans now cope with asthma, which translates into approximately 25 million people[2]. Some of the research suggests that
the increase in environmental allergies may, in fact, be one of the possible reasons for the rise in the number of people with asthma. At this time, there are various theories for the rise in the numbers, but researchers do agree that there is a definite increase in the number of Americans with this condition.
"There has been an increased prevalence of asthma in the U.S. over the past several decades," explained allergist Clifford W. Bassett, M.D., also an ACAAI fellow. "Although we may not have definitive explanations as to this increase, there are several possible theories."[3]
One of the theories that have gained a lot of support is the number of carcinogens in our atmosphere. These emanate from numerous sources such as: car pollution, industrial pollution, and cigarette smoke. There are also several key trends in the rise of asthmatic conditions which are worth noting. Research conducted in 2012 by a team of experts[4], revealed the following worthwhile information:
- Asthma prevalence increased from 7.3% in 2001 to 8.4% in 2010, when 25.7 million persons had asthma.
- For the period 2008–2010, asthma prevalence was higher among children than adults, and among multiple-race, black, and American Indian or Alaska Native persons than white persons.
- From 2001 to 2009, health care visits for asthma per 100 persons with asthma declined in primary care settings, while asthma emergency department (ED) visit and hospitalization rates were stable.[5]
Perhaps, the most notable aspect of this research is the conclusion that asthma is now at its highest level ever in the history of the condition. There is a tendency for other factors to influence the onset of asthma. These include poverty, ethnicity, race, age, and gender.
THE ROLE OF THE RESPIRATORY THERAPIST IN TREATING PATIENTS WITH ASTHMA
Given that the rates of asthma are on the rise, how can respiratory therapists work to assist their patients with this condition? Respiratory therapists play a key role in the treatment and management of people with asthma. Given that this will be a wide range of individuals with diverse needs, R.T.’s have a responsibility to stay current with treatments and research so they can offer their patients the best treatment possible. In the current healthcare environment, there has been a switch to the “disease-management paradigm”. This paradigm empowers healthcare providers and patients to manage chronic conditions, primarily from home so that there is far less need for multiple hospitalizations. When a patient can manage from home, they are more likely to feel independent and less likely to have a need for multiple practitioners.
But, the R.T. does not only see patients in their homes. In fact, they are likely to practice in a wide range of venues, and their expertise will be highly valuable. The healthcare settings that currently take advantage of the expertise of the R.T.are:
- Patient’s home
- Acute-care settings
- Long-term care residences
- Hospitals
- Out-patient clinics
- Emergency departments
The R.T. is a key member of the disease-management team. Here is an excellent definition of the disease-management paradigm:
The disease-management paradigm requires that clinicians (1) understand and consistently pursue the benefits of evidence-based medicine, (2) know and fully utilize education concepts and strategies that promote patient self-management, and (3) have the tools to measure patient outcomes and the effectiveness of the disease-management regimen.[6]
Treatment Practitioner
The R.T. plays a major role in the assessment and treatment of people with asthma. In some cases, they will be the one to actually make the diagnosis. They will then refer the patient back to their G.P. to discuss medication options. While the R.T. does not prescribe the medications, they do understand them, and they will be able to assist the patient in understanding them as well – how to take them safely, how to self-monitor, and the symptoms to look for in terms of whether or not the condition is under control. In the next section, the assessment process will be explained in more detail, but assessment of clients is an important aspect of the R.T.’s work. They will also create a detailed history of the client’s condition and their health in general. The R.T. will likely be the one to follow their progress and monitor whether or symptoms are exacerbating or abating. They will look for triggers and help the patient learn how to control them.
The R.T. is a part of an overall healthcare team in the treatment of asthma. As they are specialists in the understanding of how the human breathing mechanism functions they can provide a unique perspective for the patient. R.T.’s are a key resource and an integral part of any healthcare team. They will usually be consulted very early in the process, and doctors may well defer to them given their specialized and unique knowledge. R.T.’s should be included in all team meetings regarding a patient with asthma, and they will likely be responsible for giving specific recommendations. The R.T. plays an essential role in the treatment of a patient with asthma due to their knowledge of asthma medications, use of peak flow meters and spacers, and asthma trigger reduction.
It will be the role of the R.T. to come up with the PATIENT ASTHMA ACTION PLAN. These are given to patients, and they’re encouraged to take copies to their G.P. when they go for follow-up visits.
Here is an excellent ASTHMA ACTION PLAN[7]:
THE GREEN ZONE - I AM SYMPTOM FREE
- I have no symptoms
- I have no cough, wheeze, chest tightness or shortness of breath
- I do not cough or wheeze when I exercise or sleep
- I can do all my usual activities
- do not need to take days off work
| To Remain Symptom Free I Take These Medications | ||
| Medication | How Much to Take | When to Take It |
THE YELLOW ZONE
- I cough, wheeze, have chest tightness or shortness of breath during the day, when I exercise, or sleep
- I feel like I am getting a cold or the flu
- I need to use my reliever inhaler more than three times a week for my asthma symptom
I Need to Either Increase My Controller Medication, or Add On Another Controller
- Take _____________________2 puffs, every ________ hours as needed
(reliever)
- Increase _______________ to ________day, for ______ days, or until back in the Green Zone
(controller)
If no improvement in _____ hours, call the Doctor
THE RED ZONE – I AM IN DANGER AND NEED HELP
Any of the following:
- I have been in the Yellow Zone for 24 hours
- My asthma symptoms are getting worse
- My reliever does not seem to be helping I can not do any type of activity
- I am having trouble walking or talking
- I feel faint or dizzy
- I have blue lips or fingernails I am frightened
- This attack came on suddenly
Go Directly to the Nearest E.R. or Hospital
- Call 911
- While waiting take 2 puffs of ___________ every 10 minutes
(reliever inhaler)
Here are downloadable ASTHMA ACTION PLANS:
- http://www.nhlbi.nih.gov/files/docs/public/lung/asthma_actplan.pdf
- file:///C:/Users/User/Downloads/2778.pdf
- http://www.cheo.on.ca/uploads/asthma/files/asthma_action_plan.pdf
- A Great Action Plan for Children with Asthma: http://getasthmahelp.org/documents/aafa-childcare.pdf
Patient Educator
One of the primary roles of the R.T. is as a Smoking Cessation Consultant. Smoking is a huge risk factor for people with asthma, and in this role, the R.T. helps the patient understand the importance of smoking cessation.
In fact, they engage in this form of education with all patients who have lung disorders.
R.T.’s will also find and utilize appropriate literature to assist their patients to understand their condition. The use of illustrated texts (books and articles) is especially helpful when teaching patients how to use inhalers. Teaching and reinforcing optimal inhaler technique is essential. The R.T.’s will use the key points to serve as reminders on how to use them safely. They will also find materials in other languages so that their patients can fully understand all the material. The R.T. is in the best position to work with a patient on an ongoing basis to ensure they understand all aspects of their condition. There is additional and detailed information on patient education in the next section.
Patient Advocate
R.T.’s have the ability to advocate on behalf of their patients. In many cases, they will work with a Case Manager. This is likely to be a Social Worker. In the instance that a patient can’t afford medication, the Case Manager will work to find a drug assistance program, alternative drugs, and other important resources. The R.T. will likely work closely together with them to ensure the patient gets their medication, otherwise the condition can get out of control.
In the role of advocate, the R.T. will do this?
- The respiratory therapist embraces a patient-centered and holistic approach to care.
- The respiratory therapist takes a proactive approach to the delivery of care.
- The respiratory therapist helps patients understand and navigate the health care system.
SUMMARY
Self-management of asthma is crucial, and RTs can help patients and families develop the knowledge and techniques to achieve asthma control, avoid asthma triggers, and correctly handle worsening asthma symptoms, with minimal disruption of normal life. The RT is a key member of the asthma disease-management team.[8]
THE COMPONENTS OF A COMPREHENSIVE DISEASE MANAGEMENT PROGRAM
There are four basic components to the work of the R.T. in asthma management[9].

Assessment:
R.T.’s have the expertise to assess and diagnose an individual for asthma. This is, in fact, one of their primary roles. They follow a basic protocol in order to assess individuals and ensure that the diagnosis is accurate, so that the patient is treated accurately and appropriately. In this role, the R.T. will take an accurate record of the patient’s symptoms and ensure that asthma is the correct diagnosis. They will assess their breathing ability and monitor this in order to gain an accurate understanding of whether or not the patient has asthma, or may be at risk for the disease. The risk factors the R.T. should look for in this stage are;
Symptoms occur or worsen in the presence of[10]:
- Exercise
- Viral infection
- Animals with fur or feathers
- House-dust mites (in mattresses, pillows, upholstered furniture, carpets)
- Mold
- Smoke (tobacco, wood)
- Pollen
- Changes in weather
- Strong emotional expression (laughing or crying hard)
- Airborne chemicals or dusts
- Menses Symptoms occur or worsen at night, awakening the patient
Control of Factors:
If an individual has been correctly diagnosed with asthma, then the treatment program should begin (which will be discussed in more detail in the next section). The patient must also be monitored which is a major aspect of the R.T.’s role. The R.T. has the flexibility (depending on where they work) to go into the community, or work with patients in an out-patient or community clinic to ensure the condition is being managed in a positive way. The R.T. also has the role of explaining the condition to the patient, helping them understand their condition, give them various options for how to manage the condition, and help them to limit the risks (such as smoking) so that the condition doesn’t deteriorate. The R.T. will also explain to the patient the steps they can take to manage the condition and the various practitioners they can work with. R.T.’s will always advise the patient to be in regular contact with their G.P. so that the doctor can advise them of any factors which could possibly make their asthma worse. Additional factors the R.T. will advise the client to monitor could include the following[11]:
- Smoking
- Sinusitis
- Rhinitis
- Occupational hazards
- Dander or other allergens in the home
- Viral or other respiratory infections
A highly valuable role for the R.T. is support in smoking cessation. This is where the R.T. can truly excel as the diagnosis of asthma is an excellent reason for the R.T. to step in and encourage the patient to quit smoking. They can provide excellent information on different strategies to stop smoking, how they will or won’t interact with their medications, and offer the kind of support a patient requires to quit smoking permanently. The R.T. can also provide the patient with education on the risks they face if they continue to smoke and cope with asthma at the same time.
Pharmacologic Therapy:
Another key role for the R.T. is to explain the various levels of the condition. In this role, the R.T. should adhere to the following guide[12]:
- Mild to Intermittent: Symptoms less than twice a week, brief exacerbations, intensity may vary
- Mild Persistent: Symptoms more than twice a week but less than once a day, exacerbations may affect activity
- Moderate Persistent: Daily symptoms, daily use of inhaler, exacerbations affect activity (at least twice/week)
- Severe Persistent: Continual symptoms, limited activity, frequent exacerbations
Inhaled corticosteroids are the most common anti-inflammatory medications being used today for people with asthma. These ARE NOT prescribed by the R.T. but rather by the family doctor. When a physician makes the decision to prescribe medication they do so based on the severity of the patient’s symptoms. Again, the above guide will serve to aid the G.P. in making these decisions. The needs and symptoms of the patient will aid the doctor and the R.T. should be informed of this decision so that they, in turn, can help the patient understand their treatment, especially if there is any confusion.
Pharmacologic management is one of the keys to controlling the symptoms of asthma. It is also one of the most important as it is often used on a daily basis. Therefore, the R.T. will continue to work with the patient in order to help them understand the ways in which daily medication can affect their lives. The specific role of the R.T. will be to:
- Monitor the patient’s use of the medication
- Monitor the patient’s reactions to the medication
- Monitor the ways in which the medication is, or isn’t helping with symptom control
- Monitor any affects or contraindications to the medication
- Monitor the patient’s intake of other medications and any possible interactions with the asthma medication
- Monitor the ways in which the patient copes with their condition and adheres to program management
- Monitor any possible exacerbations of the condition
- Monitor the patient for (possible) long-term effects with asthma medications
- Monitor the need to communicate with the patient’s other treatment practitioners
Patient Education:
- The practice of respiratory therapy will continue to expand into areas where the greatest possible benefits to patients can be realized.
- The respiratory therapist is involved in the provision of a continuum of care from critical care to acute care to home care as well as in disease prevention and the education of patients.
- The respiratory therapist recognizes that a collaborative approach to patient care is fundamental in optimizing health outcomes.
- In the practice of respiratory therapy, education begins immediately upon patient diagnosis
- Basic facts about asthma
- Basic facts about the medications
- Correct use of aerosol delivery devices (i.e. Inhalers)
- How to self-monitor
- Environmental control measures
- Understand the patient’s cultural beliefs, values, and norms and incorporate those beliefs into the patient education and disease management programs
- Family education and support
The basic principles of early home care[13]:
- Prepare a written action plan to guide patient self-management, especially for patients with moderate-to-severe persistent asthma and any patient with a history of severe exacerbations.
- Recognize signs of worsening asthma (including worsening PEF) and signs that indicate the need to call the doctor or seek emergency care.
- Initiate prompt use of short-acting inhaled beta2-agonists (2 to 4 puffs every 20 minutes for 1 hour) and, for moderate-to-severe exacerbations, the addition of oral steroids.
- Monitor response to medication.
- Remove or withdraw the patient from allergens or irritants that precipitated the exacerbation
Risk Factors for Death from Asthma:
In the management of a patient with asthma the R.T. must always be aware that certain factors place a patient at risk for death. Some of these are[14]:
- Past history of sudden severe exacerbations
- Prior intubation for asthma Prior admission for asthma to an intensive care unit
- Two or more hospitalizations for asthma in the past year
- Three or more emergency care visits for asthma in the past year
- Hospitalization or an emergency care visit for asthma within the past month
- Use of >2 canisters per month of short-acting inhaled beta2-agonist
- Current use of systemic corticosteroids or recent withdrawal from systemic corticosteroids
- Difficulty perceiving airflow obstruction or its severity
- Co-morbidity, as from cardiovascular diseases or chronic obstructive pulmonary disease Serious psychiatric disease or psychosocial problems
- Low socioeconomic status and urban residence
- Illicit drug use
- Sensitivity to Alternaria
THE CURRENT TREATMENTS FOR PEOPLE WITH ASTHMA
As discussed at the beginning of this course, asthma is a condition with no cure. Therefore, the focus is on patient management. The medications used are meant to increase the air that enters the patient’s breathing passages, both on a long-term and acute basis. For some patients, there is a need for ongoing use of the medication, and there are new medications that become available as they are approved by the FDA. The primary treatment focus on asthma is the following[15]:
- Prevent chronic and troublesome symptoms, such ascoughing and shortness of breath
- Reduce your need for quick-relief medicines
- Help you maintain good lung function
- Let you maintain your normal activity level and sleep through the night
- Prevent asthma attacks that could result in an emergency room visit or hospital stay
There are two primary forms of medication in the treatment of asthma:
- Long-term control
- Quick-action relief
Each of these medications provides a different but inter-related purpose. In the case of long-term control, the purpose is to reduce airway inflammation and prevent asthma symptoms. In the case of quick-action relief, the purpose is to relieve the symptoms during a flare-up.
Medications are chosen for the person depending on a number of factors:
- The type and severity of their asthma
- The age of the patient
- The presence of co-morbidity
- The use of other prescription or alternative medications
Asthma control can and will vary over time. The use of these medications may also change over time depending on the specific needs of the patient. People respond in their own individual way which is why they each need their own action plan. People who are exposed to certain factors, for example, occupational hazards, may find that their asthma is exacerbated. Then, there are people who won’t or can’t seem to quit smoking, and this can greatly aggravate their asthma. Medications may need to be changed, or the dosage may need to be increased depending on the severity of the symptoms. This is for the patient to discuss with their doctor, but also their R.T. Medication adjustment is common in the treatment of asthma, which is why it’s crucial for patients to be educated on the risk factors for their condition.
Treatments for Asthma[16]:
For long-term treatment:
- Long-acting beta-agonists. A beta-agonist is a type of drug called a bronchodilator, which opens your airways.
- Leukotriene modifiersblock chemicals that cause inflammation.
- Mast cell stabilizers curb the release of chemicals that cause inflammation.
- Theophyllineis a bronchodilator used to prevent nighttime symptoms.
- An immunomodulatoris an injection given if you have moderate to severe asthma related to allergies that doesn’t respond to inhaled certain drugs.
The Mayo Clinic[17] lists the following as the most commonly prescribed and most effective long-term medications for the treatment of asthma:
These anti-inflammatory drugs are the most effective and commonly used long-term control medications for asthma. They reduce swelling and tightening in the patient’s airways. The individual may need to use these medications for several days to weeks before they reach their maximum benefit. Inhaled corticosteroids include:
- Fluticasone (Flovent Diskus)
- Budesonide (Pulmicort)
- Mometasone (Asmanex Twisthaler)
- Beclomethasone (Qvar)
- Ciclesonide (Alvesco)
Leukotriene modifiers
These medications block the effects of leukotrienes, immune system chemicals that cause asthma symptoms. Leukotriene modifiers can help prevent symptoms for up to 24 hours. Examples include:
- Montelukast (Singulair)
- Zafirlukast (Accolate)
- Zileuton (Zyflo)
Long-acting beta agonists (LABAs)
These bronchodilator (brong-koh-DIE-lay-tur) medications open up narrowed airways and reduce swelling. Their effects last at least 12 hours, and they're used to control moderate to severe asthma and to prevent nighttime symptoms. LABAs are used on a regular schedule along with inhaled corticosteroids. Although they're effective, they've been linked to severe asthma attacks. For this reason, LABAs are taken only in combination with an inhaled corticosteroid. Examples of LABAs include:
- Salmeterol (Serevent)
- Formoterol (Foradil, Perforomist)
Combination inhalers: Corticosteroids and long-acting beta agonists
Some inhaled asthma medication combinations contain both a corticosteroid and a bronchodilator:
- Fluticasone and salmeterol (Advair Diskus)
- Budesonide and formoterol (Symbicort)
- Mometasone and formoterol (Dulera)
For quick-relief[18]:
- Anticholinergics: Inhibit muscarinic cholinergic receptors and reduce intrinsic vagal tone of the airway. Ipratropium bromide provides additive benefit to short-acting beta-agonist (SABA) in moderate-to-severe asthma exacerbations. May be used as an alternative bronchodilator for patients who do not tolerate SABA.
- Short-acting beta2-agonists (SABAs): Albuterol, levalbuterol, and pirbuterol are bronchodilators that relax smooth muscle. Therapy of choice for relief of acute symptoms and prevention of EIB.
- Systemic corticosteroids: Although not short acting, oral systemic corticosteroids are used for moderate and severe exacerbations as adjunct to SABAs to speed recovery and prevent recurrence of exacerbations
CURRENT RESEARCH TRENDS IN ASTHMA
As with all major conditions, there is a great deal of research currently taking place. There are Asthma societies and foundations that sponsor continuous research, private foundations which grant doctors and other medical researchers with funds to engage in specific kinds of research, and major organizations such as The Center for Disease Control which are constantly engaged in trying to find cures for major ailments. In the field of asthma research, here are some of the major projects taking place.
In the United States, the Asthma Research Center[19] which is located in Brigham and Women’s Hospital is engaged in a number of asthma-related research projects:
Best African American Response To Asthma Drugs (Bard)
African Americans suffer a disproportionate burden of asthma morbidity compared to the general population, along with more asthma-related urgent care visits and higher rates of hospitalizations. It is known that African American/Black people with asthma sometimes don’t get better when they take the usual dose and type of medications like inhaled corticosteroids (“inhaled steroids”) used commonly to treat asthma.
Investigating The Role Of The Pin1 Molecule And Asthma- Pin1 Study
Recently, the global prevalence and mortality of asthma have been rising sharply. Inhaled corticosteroids remain the most effective form of asthma treatments. Despite the overall effectiveness of these asthma treatments, some concerns have been raised concerning these treatments. These concerns revolve around the side effects and compliance with some children, adolescents and a significant sub-group of asthmatic patients who either respond poorly, or not at all to these treatments.
Severe-Asthma Research Program
This research study uses a medication that is approved by the Food and Drug Administration (FDA) but not to treat asthma or AERD. The medication, prasugrel (Effient®), is an inhibitor of platelets, which we believe play a role in AERD.
Flexibility and Strength Training in Asthma
Resistive flexibility and strength training (RFST) is a new physical therapy technique that has addressed abnormalities in the arms, legs, and back. We are doing this research study to see if RFST directed to the muscles of the chest will help improve asthma symptoms by stretching the muscles around the chest.
The MRC-Asthma UK Centre in Allergic Mechanisms of Asthma[20]
- IgE function, structure and regulation:IgE is the natural antibody produced by the body as part of our defence against allergens and initiate allergic reactions in our airways, skin or gut lining. Building an accurate model of the IgE antibody and observing its interactions with other molecules and cells will help us understand how we can develop new drugs to stop the IgE antibody starting an allergic reaction.
- Leukocyte trafficking, inflammation and airway structure:White blood cells play a key role in causing inflammation when we are exposed to allergens. By tracking the movement of white blood cells through blood and tissue we can better understand how and when allergic inflammation and structural changes occur in the airways.
- Immunomodulation:Building a better understanding of how the immune cells regulate allergies and asthma, will help determine new or more effective ways to dampen down our reaction to allergens such as the treatment of allergic asthma with allergen desensitisation, also known as immunotherapy.
- Infections:One in ten children have asthma, and viral infections such as the common cold trigger up to 80% of childhood asthma attacks. Bacterial infections also pose a risk to children and adults with asthma, therefore it is important to investigate the link between bacterial and viral infections and the development of asthma.
- Identification of risk factors:In addition to hay fever and eczema, a small number of people with asthma also experience allergies to foods such as peanuts, which can present a serious health risk if poorly managed. By tracking and observing our exposure to food allergens in early life we may better understand the key genetic and environmental risk factors that lead to the development of asthma and how these could be controlled.
At New York University:
The Pulmonary Division of New York University and Bellevue Hospital have an active clinical and translational research program in asthma and airways diseases under the direction of Dr. Joan Reibman, and Dr Linda Rogers. The clinical program is focused at the longstanding Bellevue Hospital Asthma Clinic, a program of over 3,000 adults, most with moderate-severe persistent asthma. Research areas include epidemiology, physiology, genetics and immunology as well as clinical trials in asthma management. These studies include epidemiologic studies performed in collaboration with the Department of Environmental Medicine to understand the role of pollution and asthma control, physiologic studies to characterize physiologic correlates of longstanding asthma and distal airways disease.
In summary, the primary trends in asthmatic research are the need to find an actual cause for the onset of the condition, newer medications which can provide greater relief and help to keep people symptom-free, and medications to provide relief for people who are in a “the red zone”, or in a crisis situation. These are only a few of the programs currently taking place. There is also a need to understand why specific people acquire asthma and others don’t even when they have some of the same risk factors. This is where genetic research has become so valuable. The results of these kinds of studies will enable doctors and respiratory therapists to treat their patients so much more effectively. There is also a need to continue researching more effective ways of treating children with asthma, as opposed to adults. Children need to be treated differently, and newer more effective protocols are always a crucial aspect of any research program. Countries will differ in their priorities, but one commonality seems to be in place; asthma is on the rise. As other conditions are under control, the incidents of asthma continue to increase. Therefore, a greater understanding of the condition is warranted, as are more effective treatments.
[1] http://www.cdc.gov/asthma/faqs.htm
[2] http://www.healthline.com/health-news/children-allergies-and-asthma-on-the-rise-110813
[3] http://www.healthline.com/health-news/children-allergies-and-asthma-on-the-rise-110813
[4] Lara J. Akinbami, M.D.; Jeanne E. Moorman, M.S.; Cathy Bailey, M.S.; Hatice S. Zahran, M.D.; Michael King, Ph.D.; Carol A. Johnson, M.P.H.; and Xiang Liu, M.Sc
[5] http://www.cdc.gov/nchs/data/databriefs/db94.htm
[6] http://rc.rcjournal.com/content/53/6/770.full.pdf
[7] http://www.asthma.ca/adults/control/pdf/AsthmaActionPlan_ENG.pdf
[8] http://rc.rcjournal.com/content/53/6/770.full.pdf
[9] http://msdh.ms.gov/msdhsite/_static/resources/2105.pdf
[10] http://msdh.ms.gov/msdhsite/_static/resources/2105.pdf
[11] http://msdh.ms.gov/msdhsite/_static/resources/2105.pdf
[12] http://msdh.ms.gov/msdhsite/_static/resources/2105.pdf
[13] http://msdh.ms.gov/msdhsite/_static/resources/2105.pdf
[14] http://msdh.ms.gov/msdhsite/_static/resources/2105.pdf
[15] http://www.nhlbi.nih.gov/health/health-topics/topics/asthma/treatment
[16] http://www.webmd.com/asthma/guide/asthma-medications#1
[17] http://www.mayoclinic.org/diseases-conditions/asthma/in-depth/asthma-medications/art-20045557
[18] http://getasthmahelp.org/quick-relief-medications.aspx
[19] http://www.asthmabwh.org/current-studies/
[20] http://www.asthma.org.uk/research-centres

