
Atelectasis 101 2.0 CE Hours
Course Objectives:
- Describe the classification of atelectasis.
- List the causes of atelectasis
- Explain the presentation of a patient with atelectasis
- Discuss the management of patients with atelectasis.
- List the type of drugs used to manage atelectasis.
Abstract
Atelectasis is a Greek word meaning incomplete expansion. Clinically atelectasis is used to define “decreased volume” in one segment or the entire lung lobe. Atelectasis is a very common feature seen on chest x-rays in patients who are hospitalized. It is important to be aware that atelectasis has several causes. Classically atelectasis is divided in non-obstructive and obstructive. Some degree of atelectasis is a well-known complication in patients who undergo upper abdominal and thoracic surgery. In addition, use of general anesthesia and surgical manipulation of the lungs/diaphragm can also contribute to atelectasis by inducing diaphragm dysfunction and decreasing surfactant activity. The classical treatments for atelectasis include chest physiotherapy, bronchodilators, nebulized dornase Alfa (DNase), and, possibly, fiberoptic bronchoscopy.
Atelectasis is a Greek word meaning incomplete expansion. Clinically atelectasis is used to define “decreased volume” in one segment or the entire lung lobe. Atelectasis is a very common feature seen on chest x-rays in patients who are hospitalized. It is important to be aware that atelectasis has several causes. Classically atelectasis is divided in non-obstructive and obstructive.
Obstructive atelectasis
The most common type of atelectasis is obstructive and this occurs as a result of resorption of gas from the alveoli when communication between the alveoli and trachea is obstructed. The obstruction may occur at any levels of the tracheobronchial tree. Common causes of atelectasis include tumor, mucus plugs and foreign bodies. Not all people develop atelectasis at the same rate. The speed of development of atelectasis depends on the composition of inspired gas and extent of any collateral ventilation. If the lobar bronchus is obstructed, the lobe may collapse; if a segment is blocked, there may be segmental collapse. However, there is always some degree of collateral ventilation within segments and lobes and the pattern of atelectasis depends on the collateral ventilation.
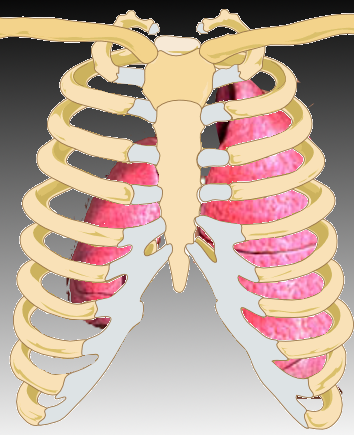
Figure 1 showing a gross anatomical view of complete right lung collapse.
Nonobstructive atelectasis
Atelectasis can also be nonobstructive and be caused by several mechanisms-
- There may be loss of between the parietal and visceral pleura. In the presence of a pneumothorax or a pleural effusion, there is no contact between the visceral and parietal pleura
- Relaxation or passive atelectasis results when a pleural effusion or a pneumothorax eliminates contact between the parietal and visceral pleurae. Generally, the uniform elasticity of a normal lung leads to preservation of shape even when volume is decreased. The different lobes also respond differently, eg, the middle and lower lobes collapse more than the upper lobe in the presence of pleural effusion, while the upper lobe is typically affected more by pneumothorax.
- External compression. Any space-occupying lesion of the chest cavity can cause compression atelectasis. The mass compresses the lung parenchyma and forces air out of the alveoli.
- Loss or insufficient surfactant. Absence of surfactant leads to adhesive atelectasis. The presence of surfactant in the alveoli normally lowers the surface tension, thus lowering the tendency of these structures to collapse. When there is decreased surfactant production or it is inactivated, this leads to instability and collapse of alveoli. This is specifically observed in patients with acute respiratory distress syndrome and other related disorders.
- Replacement of parenchymal tissue by scarring or infiltrative disease. In the presence of severe lung scarring, cicatrization atelectasis can occur as a result of decreased volume. Common causes of cicatrization include necrotizing pneumonia and granulomatous disease. Replacement atelectasis occurs when the alveoli of an entire lobe are filled by tumor (eg, bronchoalveolar cell carcinoma), resulting in loss of volume.
Middle Lobe Syndrome
A rare disorder associated with fixed or recurrent atelectasis is middle lobe syndrome. This syndrome affects the right middle lobe and/or lingula. It may be as a result of external bronchial compression by adjacent lymph nodes or by an intraluminal mass. Rarely, the middle lobe syndrome may occur in the presence of a patent lobar bronchus without any obvious obstruction. Some non-obstructive causes of middle lobe syndrome are thought to occur as a result of inflammation or defects in the bronchial anatomy and lack of collateral ventilation.
In children, it is important to be aware of this syndrome and prompt use of the fiberoptic bronchoscope with lavage may help prevent the long term adverse consequences of bronchiectasis. Bronchiectasis, in turn, may be the cause of recurrent lung infection and eventually has an unfavorable outcome in patients with chronic atelectasis.
The rheumatologic disorder, Sjögren syndrome, is known to cause middle lobe syndrome. Transbronchial biopsy in these patients often reveals presence of lymphocytic bronchiolitis in the atelectatic lobes. The atelectasis is known to respond to corticosteroid therapy suggesting that an inflammatory reaction may be responsible for the middle lobe syndrome.
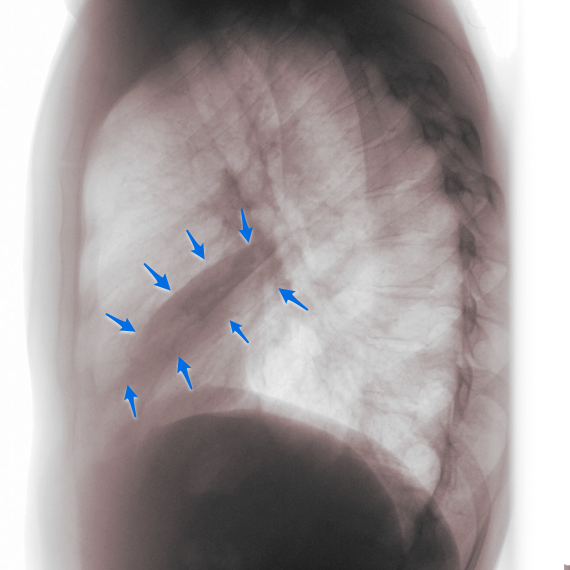
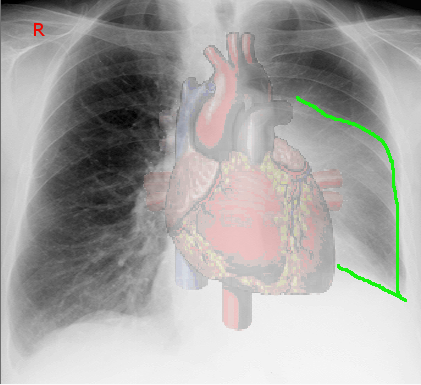
Figure 2 showing a lateral x-ray of a patient with right middle lobe collapse.
Rounded Atelectasis
In some patients with exposure to asbestos, rounded atelectasis may develop. This involves folding of the atelectatic lung due to adhesions and fibrous bands to the visceral pleura. An estimated ¾ of patients with asbestosis may develop rounded atelectasis, chiefly due to the high incidence of pleural disease. Most patients are in the 6th decade of life and often have no symptoms. Rounded atelectasis is often confused for a malignancy. The classic feature on x-ray is the talon or comet tail sign.
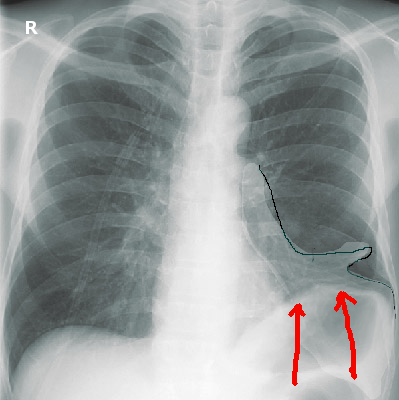
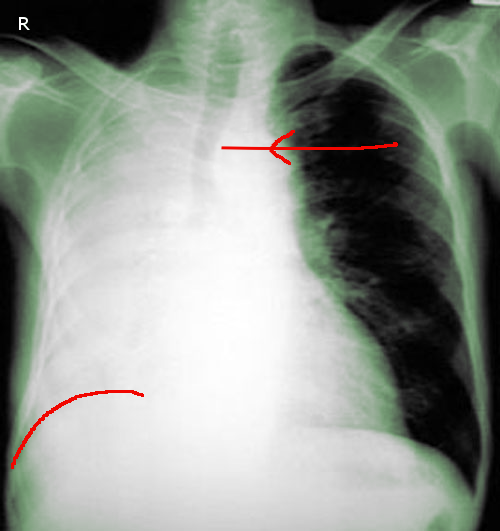
Figure 3 showing an x-ray of a patient with left lower lobe collapse. Note elevation of diaphragm
Platelike Atelectasis
Subsegmental or discoid atelectasis is often referred to as platelike atelectasis. It is commonly visualized on X-ray and is most likely due to obstruction of a small bronchus. It may be observed in people with hypoventilation, lower respiratory tract infection of pulmonary embolism. Small areas of atelectasis occur due to inadequate local ventilation and abnormalities in surfactant synthesis due to ischemia, hypoxia, hyperoxia or exposure to certain toxins. Some patients may develop mild to moderate problems in gas exchange as a result of an intrapulmonary shunt and ventilation-perfusion mismatch.
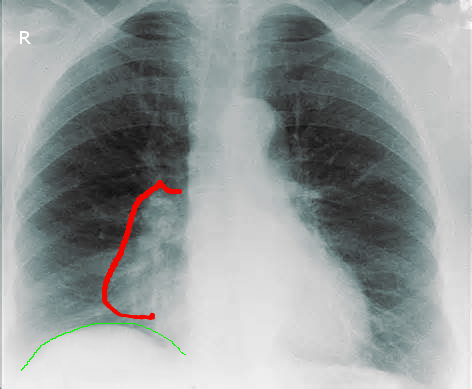
Figure 4 showing right middle lobe collapse in a patient with hilar adenopathy.
Postoperative Atelectasis
Some degree of atelectasis is a well-known complication in patients who undergo upper abdominal and thoracic surgery. In addition, use of general anesthesia and surgical manipulation of the lungs/diaphragm can also contribute to atelectasis by inducing diaphragm dysfunction and decreasing surfactant activity. Post-surgical atelectasis is usually in the basilar segments. When severe it can decrease both lung and end expiratory lung volumes. Studies show that inducing lung recruitment maneuvers followed by PEEP in post-surgical patients can decrease atelectasis and improve oxygenation.
Figure 5 shows complete right lung collapse in a post operative patient. Note trachea has shifted to the side of the collapse.
Pathophysiology
The mechanism of obstructive and nonobstructive atelectasis is quite different and is determined by several factors.
Obstructive atelectasis
Following obstruction of a bronchus, the blood circulating in the alveolar-capillary membrane absorbs the gas from alveoli. This process can lead to collapse of the lung and an airless state within those alveoli in a matter of several hours. In the early stages, blood then perfuses the unventilated lung. This results in a shunt and, potentially, arterial hypoxemia. Subsequent to obstruction of a bronchus, filling of the alveolar spaces with secretions and cells may occur, thereby preventing complete collapse of the atelectatic lung. The uninvolved surrounding lung tissue distends, displacing the surrounding structures. The heart and mediastinum may shift toward the atelectatic area, the diaphragm may become elevated, and the chest wall flattens.
If the obstruction to the bronchus is removed, any complicating post obstructive infection subsides and the lung returns to its normal state. If the obstruction is persistent and infection continues to be present, fibrosis and/or bronchiectasis may develop.
Nonobstructive Atelectasis
The loss of contact between the visceral and parietal pleurae is the primary cause of nonobstructive atelectasis. A pneumothorax or a large pleural effusion can induce passive or relaxation atelectasis. Pleural effusions tend to affect the lower lobes, whereas pneumothorax tends to affect the upper lobes. Presence of a moderate size pleural effusion/mass or lung mass can decrease lung volume by compressing the lung.
Lack of surfactant is known to cause adhesive atelectasis. The surfactant has phospholipid dipalmitoyl phosphatidylcholine, which prevents lung collapse by reducing the surface tension of the alveoli. Lack of production or inactivation of surfactant, which may occur in acute respiratory distress syndrome (ARDS), radiation pneumonitis, and blunt trauma to the lung, cause alveolar instability and collapse.
Middle lobe syndrome (recurrent atelectasis and/or bronchiectasis involving the right middle lobe and/or lingula) has recently been reported as the pulmonary manifestation of primary Sjögren syndrome.
Scarring of the lung parenchyma leads to cicatrization atelectasis.
Replacement atelectasis is caused by filling of the entire lobe by a tumor such as bronchoalveolar carcinoma.
Causes
The major causes of acute or chronic atelectasis are related to bronchial obstruction that may be caused by the following:
- Aortic aneurysm compressing the bronchi and/or inducing distortion of bronchus
- Endobronchial tumors
- Foreign bodies
- Mucus plugs of tenacious sputum
- External compression by a tumor, a lymph node, or external pulmonary compression by pleural fluid (effusion) or air (pneumothorax) may also cause atelectasis.
Absence or lack of adequate surfactant production can also cause alveolar collapse and result in atelectasis. This is commonly seen in patients with ARDs and oxygen toxicity
Resorptive atelectasis is caused by the following:
- Aspirated foreign body
- Bronchogenic carcinoma
- Bronchial obstruction from metastatic neoplasm (e.g., adenocarcinoma of breast or thyroid, hypernephroma, melanoma)
- Extrinsic compression of an airway by neoplasm, lymphadenopathy, aortic aneurysm, or cardiac enlargement
- Inflammatory etiology (e.g., tuberculosis, fungal infection)
- Mucous plug
- Malpositioned endotracheal tube
Relaxation atelectasis is caused by the following:
- A large emphysematous bulla
- Pleural effusion
- Pneumothorax
Compression atelectasis is caused by the following:
- Chest wall, pleural, or intraparenchymal masses
- Loculated collections of pleural fluid
Adhesive atelectasis is caused by the following:
- Acute respiratory distress syndrome
- Cardiac bypass surgery
- Hyaline membrane disease
- Prolonged shallow breathing
- Smoke inhalation
- Uremia
Cicatrization atelectasis is caused by the following:
- Idiopathic lung fibrosis
- Chronic tuberculosis
- Fungal infections like histoplasmosis
- Radiation induced fibrosis
Replacement atelectasis is caused by alveoli filled by tumor or fluid.
Right middle lobe syndrome (also known as Brock syndrome) refers to recurrent right middle lobe collapse secondary to airway disease, infection, or a combination of the two. The right middle lobe bronchus is long and thin. The angle of the lobe also does not permit effective drainage or clearance of secretions. This often leads to retention of mucus and other debris. The middle lobe bronchus can also be compressed by lymph nodes. While some individuals with middle lobe syndrome are often asymptomatic, many will present with recurrent productive coughing episodes and a long history of right-sided lung infections.
Rounded atelectasis is caused chiefly by uremic pleuritis and asbestos-related pleural disease.
Figure 6 showing left lower lobe collapse in a patient with a bronchial carcinoid. Note elevation of left hemidiaphragm
Epidemiology
Postsurgical atelectasis is a common problem after many types of surgical procedures. In most post-surgical atelectasis, lobar atelectasis is commonly seen. Unfortunately the prevalence of post-surgical atelectasis is not known because data are not well documented or released by most physicians and hospitals. All numbers are underestimates because in many cases the disorder is often not recognized during the early post-operative period.
Race
Post obstructive atelectasis occurs in all populations, genders and has no racial predilection. While post obstructive atelectasis can occur in anyone at any age. Most cases are seen in middle or elderly individuals. The atelectasis most commonly occurs after upper abdominal or thoracic surgical procedures.
Mortality/Morbidity
Atelectasis by itself does not carry a high morbidity. However, if the patient has other comorbidity or lung disease, the patient may not tolerate atelectasis well. Hypoxia can be moderate to severe in some patients. The majority of post-surgical atelectasis improves with supportive care. In patients with lung cancer, severe emphysema or COPD; the prognosis of post obstructive atelectasis is not always good. Often these patients need to be transferred to the ICU and receive aggressive pulmonary are or even mechanical ventilation.
Even though older literature has associated fever with post obstructive atelectasis, a recent study found no clinical evidence supporting the idea that atelectasis is always associated with early fever after surgery. Most symptoms and signs are determined by the rapidity with which the bronchial occlusion occurs and the size of lung area affected. Presence or absence of any lung infection will also influence the rate at which atelectasis develops.
In patients who have sudden occlusion of a large bronchus, this may be associated with chest pain, onset of dyspnea, and hypoxia. Other features may include fever, tachycardia, tachypnea and even shock with cyanosis. If the atelectasis is slow and gradual in development, then the patient may be asymptomatic at rest. Middle lobe syndrome is often symptomatic, although external compression may induce irritation of the airways and induce a dry hacking cough.
Physical
The physical findings in a patient with atelectasis depend on the degree of atelectasis. When the atelectasis is mild, the patient may have no obvious findings. However, moderate to large lobar atelectasis may be associated with dullness to percussion over the involved area and diminished or absent breathe sounds. Excursion of the chest on the involved hemithorax may be absent or decreased. With severe atelectasis, the mediastinum, trachea and heart may be shifted towards the affected side.
Laboratory Studies
Because atelectasis can result in hypoxemia, an arterial blood gas should be performed. The result may show a low PaO2 but the PaCO2 may be normal initially. It may be decreased in patients who are hyperventilating.
Histologic Findings
Samples obtained during bronchoscopy include washings and sometimes brushing are sent to the laboratory if there is a malignancy suspected. In most cases, there is no need to send the tissues for analysis.
Imaging Studies
The first imaging study of choice in a patient with suspected atelectasis is a chest x-ray. The x-ray may reveal displacement of the tissues and opacification of the collapsed lobe. Other features of atelectasis may include mediastinal shift towards the side of lung collapse, displacement of the hilum, elevation of the ipsilateral diaphragm and silhouetting of the diaphragm or the heart border.
Treatment
Medical Care
The treatment of atelectasis depends on the underlying etiology. For acute atelectasis including postoperative lung collapse, one needs to remove the underlying cause like a mucus plug. The classical treatments for atelectasis include chest physiotherapy, bronchodilators, nebulized dornase Alfa (DNase), and, possibly, fiberoptic bronchoscopy. The latter study may be useful in patients with mucous plugging of the airways. In patients with passive and adhesive atelectasis, positive end-expiratory pressure might be a useful adjunct to treatment.
Non-Drug Therapies
There are several non-drug therapies that can be used to help improve ability to cough and increase clearance of secretions from the airways, this include use of chest physical therapy, postural drainage, vibration and chest wall percussion.
Another technique called huffing or forced expiration is also used in alert patients. All these techniques have been evaluated in studies. The results of studies show that they all can result in increased airway clearance as assessed by sputum characteristics and clearance of radio aerosols from the lung, compared to just coughing alone.
For post-operative atelectasis, the best treatment is prevention. If possible use of anesthetic agents that are associated with post anesthesia narcosis should be withheld. Narcotics should be used sparingly because they are known to suppress the cough reflex.
Another way to prevent post-surgical atelectasis is early ambulation, while this can be accomplished in most surgical patients, some patients may not be able to get out of bed soon after surgery. Another technique that is very useful in preventing post-surgical atelectasis is use of incentive spirometry.
Other treatments include encouraging the patient to deep breathe and cough several times every hour during the waking hours. Individuals who have thick viscous section may also benefit from nebulized bronchodilator therapy. Nebulizers can help liquefy secretions and thus promote their easy removal either via a coughing.
In patients with lobar atelectasis, some patients may need aggressive chest physical therapy, which can also help mobilize secretions and help re-expand the collapse lung. When these efforts are not successful and the patient remains symptomatic, the best test of choice is flexible bronchoscopy.
Fiberoptic Bronchoscopy
The use of flexible bronchoscopy in a patient with atelectasis is both diagnostic and therapeutic. It is usually not needed in minor cases but may be of use in patients who are not improving or the cause of atelectasis is unknown. Flexible bronchoscopy can be done at the bedside and quickly determines the cause of bronchial obstruction. Flexible bronchoscopy also has therapeutic benefits as it allows for removal of mucus plugs that are causing the obstruction. However, flexible bronchoscopy has practical limitations, as the scope usually cannot reach the distal bronchial lesions.
Figure 7 showing carina during bronchoscopy. There is a large mucus plus obstruction the right main bronchus.
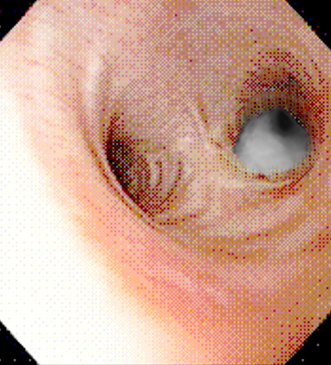
The procedure can be performed at the bedside without the use of general anesthesia. However, patients may require some topical local anesthetic to numb the oropharynx and vocal cords prior to insertion of the scope. The procedure only takes 15-20 minutes. The patient must be provided with adequate oxygen as frequent suctioning can induce hypoxia. Monitoring of the pulse oximetry is highly recommended during the procedure.
Sometimes the procedure may reveal the cause of the atelectasis, such as a cancer or a foreign body. The one advantage of fiberoptic bronchoscopy is that it can help remove thick secretions. However, routine use of fiberoptic bronchoscopy in post-surgical patients has not been demand to be more effective than deep breathing, standard chest physical therapy, coughing and suctioning.
In patients on the mechanical ventilator who are spontaneously ventilating, standard respiratory therapy techniques should be used to improve ventilation. Fiberoptic bronchoscopy should be reserved for patient in whom chest physiotherapy is contraindicated like an immobilized patient or chest trauma or in whom the procedure is not well tolerated or it is unsuccessful.
Further, in patients on the ventilator, fiberoptic bronchoscopy is only done when the patient has thick secretions and the chest x-ray reveals sign of lung collapse. The technique allows one to assess the degree of airway obstruction and determine the cause. Many studies have shown that single suction fiberoptic bronchoscopy can lead to improvement in oxygenation and immediate improvement in the chest x-ray. In some patients, repeated bronchoscopy may be required every day or every other day until improvement occurs.
Surgical Care
Surgery is never the first treatment of atelectasis. It is only used a last resort treatment in chronic cases where the lung has been damaged. Some patients may need a segmental resection of lobectomy. The procedure may be done via a thoracotomy or thoracoscopy. After surgery, aggressive chest physical therapy, incentive spirometry and ambulation are encouraged to prevent recurrence of atelectasis.
Prior to any surgery of the upper abdomen or chest, patient should be taught prophylactic maneuvers for decreasing the risk include of postoperative atelectasis in high risk patients should be encouraged. These techniques include coughing exercise, deep breathing exercise, and incentive spirometry. For maximal benefit, these prophylactic measures should be taught and started several days prior to surgery. In addition, the patient must be told about ambulation soon after surgery.
Medications
In patients with atelectasis who have difficulty coughing, bronchodilators can be used as expectorants. These agents open up the airways and improve ventilation. The classic bronchodilators used are short acting agents like beta blockers, anticholinergics, and methylxanthine.
Bronchodilators
Patients with atelectasis often benefit from bronchodilators. These agents can decrease tone in the small and large airways and enhance ventilation. Bronchodilators may be used to encourage sputum expectoration; if underlying airflow is present, these agents may also improve ventilation. Some patients may require broad-spectrum antibiotics to treat the underlying infections, which may occur because of bronchial obstruction. The classes of bronchodilators used to treat patients with atelectasis include the following:
Beta2 adrenergic agonists (albuterol sulfate [Ventolin HFA, Proventil HFA, ProAir HFA; levalbuterol [Xopenex) , pirbuterol acetate [Maxair Autohaler] relax the smooth muscle fibers of the large airways and relieve bronchospasm. These agents are used to treat bronchospasm in patients with acute symptoms of wheezing. Albuterol is one of the most common bronchodilators used and is available in multiple formulations (eg, solution for nebulization, metered-dose inhaler, oral solution). It is important for the therapist to know that prolonged use of albuterol can lead to tachyphylaxis due to receptor down regulation
Pirbuterol (Maxair Autohaler) is available as a breath-actuated or ordinary inhaler. This agent is easy to administer because of its breath-actuated device and hence it is a good choice for the treatment of wheezing in children.
Levalbuterol (Xopenex) is the nonracemic form of albuterol, levalbuterol (R isomer). At low doses, it is effective and also has fewer adverse effects like tachycardia, hyperglycemia or hypokalemia. The dose may be doubled in acute severe episodes when even a slight increase in the bronchodilator response may make a big difference in the management strategy (eg, in avoiding patient ventilation).
Anticholinergic Agents
These agents can also be used at the same time as beta adrenergics for acute exacerbations. Ipratropium (Atrovent) is an anticholinergic agent that is known to inhibit airway secretions and also dilate the airways.
Standard delivery systems and routes
Albuterol (2.5-5 mg) can be administered every 20 minutes in 3 quick doses and then 2.5-10 mg every 1-4 hours as needed; if the agent is used as a nebulizer, it is mixed with 3-4 ml of saline. Some type of compressed air or oxygen delivery is required at a rate of 6-8 L/min for nebulizer therapy. In children the dose of albuterol is 0.15 mg/kg (minimum dose 2.5 mg) every 20 minutes in three quick doses and then 0.15-0.3 mg/kg up to 10 mg every 1-4 hours as needed.
Another method to deliver beta agonists is the metered-dose inhaler (MDI), which is often used in combination with a spacer or holding chamber. The dose is 4-8 puffs every 20 minutes up to 4 hours, then every 1-4 hours as needed. One big al advantage of the MDI/holding chamber is that it requires little or no assistance from the respiratory therapist once the patient understands how to use the medication; the patient can be discharged from the ED with the same spacer and albuterol canister. This modality is especially effective in areas where patients may be unable to afford their inhaled beta agonists.
Side effects of beta agonists include a mild tachycardia and a resting tremor. However, many patients who present with acute asthma and tachycardia actually have a lowering of their heart rate with bronchodilator therapy. In addition, inhaled beta agonists are known to lower levels of potassium by an average of 0.4 mEq/L.
Some patients may not respond well to an inhaled beta agonist and in these individuals, parenteral treatment with 0.25 mg terbutaline or 0.3 mg of 1:1000 concentration of epinephrine administered subcutaneously may be of benefit. However, this treatment should be reserved for patients who are critically ill and not responding to serial treatments with inhaled beta-agonist/anticholinergic therapy and other conventional therapies.
Ipratropium 0.5 mg has had variable benefit in adults and is most effective in children and smokers with comorbid COPD. It may be combined with albuterol in patients with severe exacerbation of wheezing. Ipratropium can be administered in combination with albuterol every 20 minutes for 3 doses, then as needed. The addition of ipratropium has not been shown to provide further benefit once the patient is hospitalized.
Antibiotics
If a patient has chronic atelectasis and production of foul smelling sputum, pneumonia may be festering. Most healthcare providers will start the patient on an antibiotic. The type of antibiotic depends on the causative organism, severity of infection and susceptibility of the bacteria. The types of organisms that must be covered include Haemophilus influenza, proteus, E coli, Klebsiella and Moraxella.
Mucolytic agents
N-acetyl cysteine (Mucomyst)
N acetyl cysteine is a mucolytic agent that has the ability to breakdown disulfide bonds in mucus and liquefies it. This makes it easier to cough up the mucus. N-acetyl cysteine is often used to thin mucus in patients with abnormally thick mucus as in cystic fibrosis. The agent is often used to treat patients with bronchitis, bronchiectasis, pneumonia, cystic fibrosis, COPD and interstitial fibrosis. It is also used in post-surgical patients who have a tracheostomy. However, N -acetyl cysteine aerosol is not routinely recommended because of the risk of bronchoconstriction and the lack of documented efficacy. Some experts recommend its use limited to direct instillation at the time of fiberoptic bronchoscopy. It efficacy is still benign debated. Anecdotal case reports suggest that it may help patients with thick viscous mucus plugs.
Dornase Alfa
Dornase Alfa (Pulmozyme) is a recombinant human enzyme that can breakdown DNA. This action then allows the body’s proteolytic enzymes to then break down the proteins into smaller molecules, which decreases viscosity and reduces surface tension of purulent sputum. The sputum can then be coughed up. The agent is often used to treat patients with cystic fibrosis and bronchiectasis. It may be a useful option in some infants with atelectasis that has failed to respond to all other treatments. The down side of Dornase Alfa is the cost and hypersensitivity reactions. Dornase has been widely studied in children and shown to be effective but such data do not exist for adult patient.
Pain Medications
The amount of analgesia used in post-operative patients should be just adequate, too much analgesia and the patient may fail to take deep breaths or cough effectively. The anesthesia should be just adequate so that the patient is able to participate in chest physical therapy, cough forcefully and use incentive spirometry.
In patients who undergo thoracotomy or underlying lung disease, the use of epidural analgesia is an effective method for pain control and also helps the patient undertake chest physical therapy.
Complications
Minor atelectasis may not have any adverse effects but moderate to severe atelectasis involving a lobe may lead to the following:
- Acute pneumonia
- Bronchiectasis
- Empyema
- Hypoxemia
- Pleural effusion
- Post obstructive drowning of the lung
- Respiratory failure especially if the lung has intrinsic disease
- Sepsis
Prevention
In patients who have a weak cough or are not able to cough up secretions, place the patient in such a position that the uninvolved side is dependent to promote drainage from the affected lung. Post-operative use of incentive spirometer and deep breathing and coughing are also recommended.
Some patients may require nasotracheal suctioning if the atelectasis keeps on recurring. This is typically performed in patients with neuromuscular disease and have ineffective cough.
In patients who have fever and if a specific microorganism is isolated from bronchial secretions, a broad-spectrum antibiotic should be started. Once the culture results become available, an appropriate antibiotic that is sensitive should be used.
If there is chest x-ray evidence of post-operative atelectasis, the patient should be adequately oxygenated as this can help re-expansion of the lung segments. The amount of supplemental oxygen should be titrated to achieve arterial oxygen saturation greater than 90%
If the patient has complete lung collapse and is severely hypoxic, it is important to quickly intubate and mechanically ventilate the patient. endotracheal intubation not only provides ventilatory support and oxygenation it also provides the therapist a much easier way to suction the airways and even allows for performance of a flexible bronchoscopy, finally the positive pressure ventilation, large tidal volumes and use of PEEP can be used to re-expand the collapse lung segment or lobe.
Patients, who do not require mechanical ventilation, may benefit from continuous positive airway pressure delivered either via a facemask or a nasal cannula. This may be effective in improving oxygenation and re-expansion the lung lobe.
If the patient has signs of a fever, chill, night sweats or leukocytosis, as a result of secondary atelectasis, one must start broad-spectrum antibiotics
When there is an obstruction of a major bronchus, it may cause severe coughing. Thus, these patients should not be given antitussive medications as the cough reflex may diminish and worsen the obstruction.
References
- Field-Ridley A, Sethi V, Murthi S, Nandalike K, Li ST. Utility of flexible fiberoptic bronchoscopy for critically ill pediatric patients: A systematic review. World J Crit Care Med. 2015 Feb 4;4(1):77-88.
- Restrepo RD, Braverman J. Current challenges in the recognition, prevention and treatment of perioperative pulmonary atelectasis. Expert Rev Respir Med. 2015;9(1):97-107.
- Hartland BL, Newell TJ, Damico N. Alveolar Recruitment Maneuvers Under General Anesthesia: A Systematic Review of the Literature. Respir Care. 2014 Nov 25.
- Sobocińska M, Sobociński B, Jarzemska A, Serafin Z. Rounded atelectasis of the lung: A pictorial review. Pol J Radiol. 2014;79:203-9.
- Karim A, Arora VK. Applications of ultrasonography in respiratory intensive care. Indian J Chest Dis Allied Sci. 2014;56(1):27-31.
- Thornby KA, Johnson A, Axtell S. Dornase Alfa for Non-Cystic Fibrosis Pediatric Pulmonary Atelectasis. Ann Pharmacother. 2014;48(8):1040-1049
- do Nascimento Junior P, Módolo NS, Andrade S, Guimarães MM, Braz LG, El Dib R. Incentive spirometry for prevention of postoperative pulmonary complications in upper abdominal surgery. Cochrane Database Syst Rev. 2014 ;2:CD006058
- Sabaté S, Mazo V, Canet J. Predicting postoperative pulmonary complications: implications for outcomes and costs. Curr Opin Anaesthesiol. 2014;27(2):201-9

